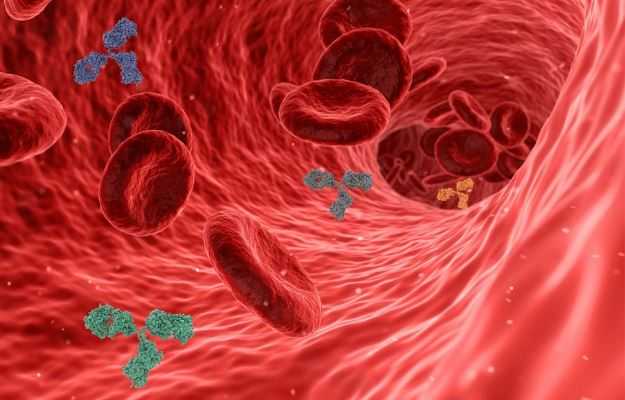
Bacteremia refers to the presence of bacteria in the blood. Blood is a sterile medium and bacteria do not generally appear in it. However, even simple acts like brushing or minor medical procedures can transiently introduce bacteria into the blood. While not all types of bacteremia are symptomatic, some can establish bloodstream infection or septicemia. The body’s immune system fights septicemia with an appropriate, and usually adequate, immune response. Sepsis is the term used to refer to the exaggerated and dysregulated immune response of the body to ward off this bloodstream infection. Such an immune response often results in widespread organ damage. Signs and symptoms of sepsis are pronounced and can often prove fatal. At times, in severe sepsis, the patient’s blood pressure can fall dangerously low causing irreparable damage by altered cellular metabolism. This is called septic shock and has a staggeringly high mortality rate.
(Read more: Bacterial infection)

 Doctors for Bacteremia
Doctors for Bacteremia