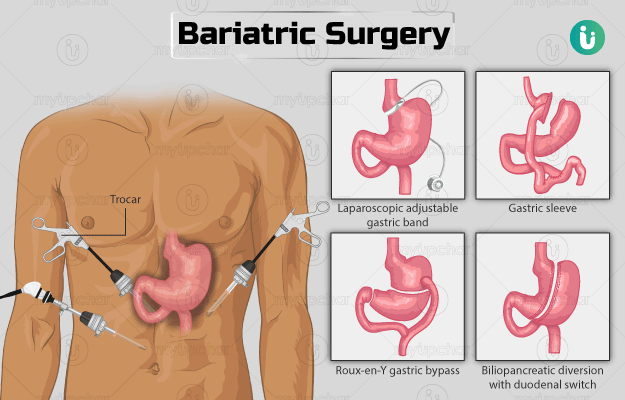
The procedure for each bariatric surgery is different. All the surgeries can be done laparoscopically as follows:
- Your healthcare practitioner will first give you general anaesthesia so that you feel sleepy and have no pain.
- The surgeon will then make one to five small cuts in your abdomen.
- Through these cuts, a tiny camera called a laparoscope and small instruments required to operate will be placed inside your belly.
Laparoscopic adjustable gastric band
The duration of LAGB is 30 to 60 minutes. After the laparoscope and instruments are placed in your stomach, the following procedure will be followed:
- The surgeon will place a band around the upper area of your stomach to separate it from the lower bottom area.
- This forms a small upper pouch with a narrow opening that enters into a larger bottom area of stomach.
- This surgery does not need stapling or cuts inside the abdomen. A small access port that is connected to the band will be placed below your skin to allow the surgeon to adjust the gastric band if it moves later. The port can be used to introduce saline into the band to increase or decrease the constriction of stomach.
Whenever you eat after the surgery, the small pouch will fill up first, and you will get a feeling of fullness with just a small quantity of food. Later, the food will slowly empty into the main part of your stomach.
You can go home on the same day after the surgery.
Gastric bypass surgery
The duration of this surgery is 2 to 4 hours. For a gastric bypass surgery, the following steps will be taken after the laparoscope and instruments are placed inside your stomach:
- Your surgeon will use a laparoscopic staple to make a small pouch from the upper part of your stomach.
- In the second step, they will connect a small portion of the jejunum (middle part of the small intestine) to the pouch made from the upper part of the stomach through a small hole.
- The incision will be closed with sutures.
When you eat after the surgery, the food will first enter the pouch and then will go into the jejunum (small intestine) through the opening between these organs. This will cause less absorption of calories while also making you eat less.
Gastric bypass surgery can be also be done as an open surgery where one large surgical cut is made in the belly).
Post-surgery care: After gastric bypass surgery, you may be asked to stay in the hospital for 1 to 4 days. In the hospital, the following things can be expected:
- On the same day of the surgery, your doctor will ask you to sit on the bedside and walk a little.
- A catheter will be inserted through your nose into your stomach to remove fluid from the intestine (which may be present due to the surgery). It may be kept in for 1 to 2 days.
- A catheter may also be inserted in your bladder to drain urine.
- You will not be able to eat anything for the first 3 days after surgery. After that, you can slowly start with liquids and then soft or pureed foods.
- You will be asked to wear special stockings on your legs to prevent blood clotting.
- Your doctor will give you medicines like pain relievers through an intravenous (IV) line or by placing a catheter into your vein.
You will be allowed to go home when:
- You do not need pain killers
- You can move around without much pain
- You can eat food without vomiting
Gastric sleeve surgery
This surgery takes 60 to 90 minutes. After the laparoscope and instruments are placed in your stomach, the following steps will be taken:
- Using a laparoscopic stapler, the surgeon will divide your stomach to form a narrow vertical sleeve or a banana-shaped stomach.
- The rest of the stomach will be removed by cutting it.
- After this, the tools and laparoscope will be removed from your body, and cuts will be closed with stitches.
The new, smaller-sized stomach will limit the quantity of food you eat, thus making you fuller soon.
You can go home within 2 days after the surgery.
Biliopancreatic diversion with duodenal switch
The BPD/DS surgery is performed in the following manner:
- The surgeon will form a smaller, tube-like pouch by cutting a part of the stomach (vertically) using a laparoscopic stapler.
- The upper portion of the small intestine (the duodenum) will be divided and connected to the bottom portion of the small intestine (duodenal switch).
- The bypassed small intestine carries the bile and pancreatic enzymes that are needed for the digestion of fats and proteins. This portion is reconnected to the last part of the small intestine (biliopancreatic diversion).
- The surgeon will remove the tools and close the cuts with stitches or surgical glue.
This surgery can also be performed as open abdominal surgery.
After the procedure, when you eat, the food goes only through the new pouch and is emptied in the end part of the small intestine. Thus, less food is digested, and fewer nutrients and calories are absorbed.
You will be shifted to the hospital room after the surgery. The healthcare provider will ask you to get out of the bed and walk a little. During the hospital stay, you will be on a liquid diet.