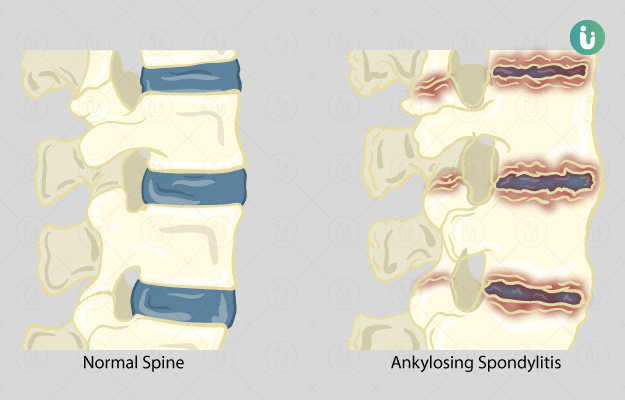
What is spondylitis?
Spondylitis is an arthritis involving the spine, in which inflammation is seen between the vertebrae (bones that form the spine) and in the joints between the spine and pelvis, along with the involvement of tendons and ligaments near the spine. It is more common and severe in men. Occasionally, other joints may also be involved.
As per the new classification, spondylitis is classified as axial spondyloarthritis (affecting the pelvis and spine) and peripheral spondyloarthritis (affecting other joints).
What are its main signs and symptoms?
The signs and symptoms of spondylitis include:
- Pain and stiffness in the ribs, buttocks, hips, lower back, shoulders, and heels.
- The range of motion of the spine is limited, which restricts mobility
- Fever and fatigue
- Eye or bowel inflammation
- Rarely, heart or lung is involved
- Pain and inflammation in the mucous membranes, skin, eyes, bladder, and genitals.
- Heel pain (enthesitis), iritis and knee swelling,
What are the main causes of spondylitis?
Although the cause of spondylitis is not clear, genetic factors are suspected to be involved. It is thought to be associated with the HLA-B27 gene; however, the mechanism remains unknown. Other factors thought to be causing spondylitis include:
- Environmental factors
- Immunological factors- autoimmunity where the body’s own immune cells attack various tissues causing inflammation
- Long lasting inflammation of the intestines
How is it diagnosed and treated?
The diagnosis of spondylitis is based on individual signs and symptoms. The following steps are carried out by the physician to confirm the diagnosis:
- Thorough history followed by a physical examination.
- X-rays, mainly of the sacroiliac joints and spine, which could confirm the diagnosis.
- Blood test to check for the HLA-B27 gene; however, its presence does not confirm the diagnosis.
Treatment of a spondylitis:
Currently, there is no known cure for spondylitis. Hence, the aim of treatment is to reduce pain and stiffness, prevent deformity and preserve function, slow down the progression of disease and help maintain posture. The treatment modalities include the following:
- Regular exercises, which involve stretching and strengthening, along with deep breathing exercises and posture exercises to prevent stooping and slumping. A physiotherapist plays an important role in developing an exercise routine.
- Treatment with medications include:
- Non-steroidal anti-inflammatory drugs (NSAIDs) which are mostly used to control symptoms.
- Steroids, which include cortisone or prednisone, are rarely used.
- Sulfasalazine or methotrexate may be used, but are less helpful for the spine disease.
- Currently, biologic anti-TNF-α agents such as infliximab, etanercept and adalimumab are in use, which helps to reduce symptoms as well as slow disease progression. They are given intravenously.
- Surgical options for ankylosing spondylitis are limited. There are no specific surgeries for the spine. However, shoulder or hip joint replacement surgery can be beneficial in severe cases.

 Doctors for Spondylitis
Doctors for Spondylitis  OTC Medicines for Spondylitis
OTC Medicines for Spondylitis