Mental health is a sum of many things: the absence of mental illness and the ability to cope with the normal stresses of life, to recognise our abilities and work productively and to relate to others and form lasting relationships, among other things.
According to India’s Mental Health Care Act 2017, “‘mental illness’ means a substantial disorder of thinking, mood, perception, orientation or memory that grossly impairs judgment, behaviour, capacity to recognise reality or ability to meet the ordinary demands of life, mental conditions associated with the abuse of alcohol and drugs, but does not include mental retardation which is a condition of arrested or incomplete development of mind of a person, specially characterised by subnormality of intelligence.”
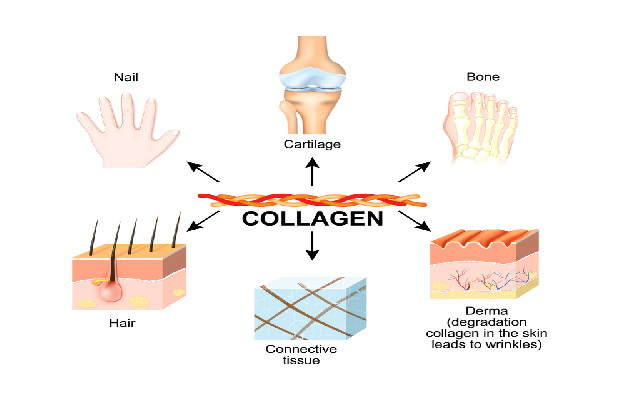
Researchers are finding more and more evidence that our mental health—how we feel, behave, think, our psychological and emotional well-being—is linked to our physical well-being and our quality of life.
While all of us may want to live a happy and healthy life, the truth is that anyone can develop a mental health condition. Genes, life events, lifestyle, our environment and circumstances—they all have an impact on our mental health.
In terms of causes of mental health issues, some disorders like Alzheimer’s disease are rooted more in physiology (build-up of tau and amyloid proteins in the brain) while others have psychological or social origins (example, social anxiety). Though scientists are now finding that the physiological and the psychological are deeply interlinked.
Mental health conditions extract a cost from the person, and from society. The World Health Organization (WHO) says: “Mental, neurological and substance use disorders make up 10% of the global burden of disease and 30% of non-fatal disease burden.” Additionally, losses to global productivity from depression and other mental health problems amount to $1 trillion a year!
The taboo around mental health issues is one of the greatest impediments to seeking proper help for them—not just in India but around the world. It’s important to separate mental health issues from moral labels for many reasons because it is as pointless to blame someone for a mental health illness as it is to hold someone responsible for getting sick. For example, research has shown that alcoholism and opioid dependency are illnesses—some people are prone to addiction at much lower thresholds. As they have no control over this addiction, mental health experts argue that it is unhelpful to see substance use as a moral failing.
Happily, we can each take greater care of our mental health—if we prioritise mental health in the same way that we take care of our physical health and take cognisance of mental health problems as and when they can occur. What makes this slightly easier now is that with each passing day, scientists are unpacking something new about brain function, brain chemistry (neurotransmitters like dopamine, acetylcholine, GABA, glutamate, serotonin, oxytocin, endorphins and norepinephrine that nerve cells use to talk to each other) and our primal instincts like fear, love and social engagement (research shows that the feeling of love may predate the development of the cerebral cortex in humans).
This article is an attempt to start a conversation about mental health, with sections on risk factors for mental health conditions, the most common mental health condition in India and the world, and some tips and tools for better mental health.