Summary
Cataracts occur when certain changes in the constitution of the eye lens cause it to become opaque and now allow light to pass through it. It develops gradually and leads to poor vision and vision loss. The removal of cataract is known as cataract surgery.
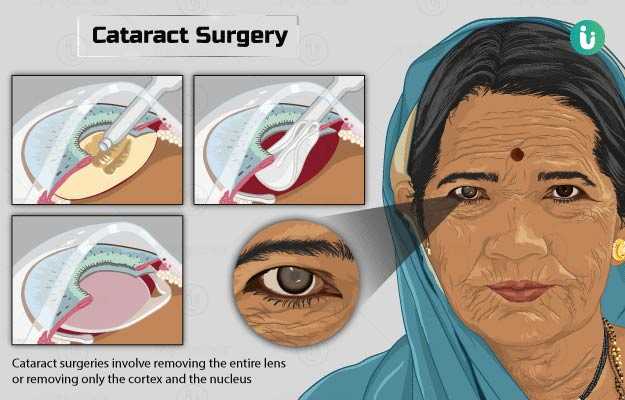
The eye lens is made up of an outer capsule, middle cortex and an inner nucleus. Depending on the region affected, cataracts can be of three types – capsular, cortical and nuclear cataracts.
Ageing is the most common reason for the development of cataracts. However, other factors that contribute to the formation of a cataract include UV ray exposure, malnutrition or other nutritional deficiencies, smoking, diabetes, and trauma.
Signs of a cataract include blurring vision, sensitivity to light, especially night glare, and colour fading.
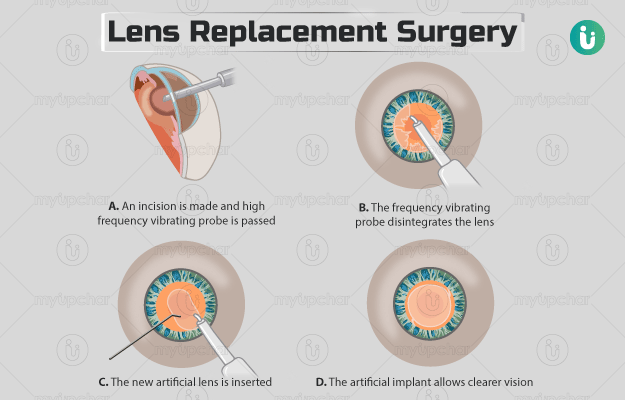
Cataract surgeries involve removing the entire lens with the outer capsule (intracapsular), removing only the cortex and the nucleus (extracapsular), and phacoemulsification (where the contents of the lens are broken down and then drawn out). The procedure may take about 30 minutes to complete, and you will be allowed to go home after the surgery.