SARS-CoV-2, the virus that causes COVID-19, has made 20 million people sick and claimed more than 736,000 deaths around the world as of 12 August 2020.
Even as many countries deal with the costs of the COVID-19 pandemic (health costs and economic costs), one question keeps coming up: is it possible to be reinfected by the new coronavirus infection after you have recovered from it once. (Read more: Can you get coronavirus infection twice?)
New research published in the journal Science on 2 July 2020 looked at the possibility of reinfection, in rhesus macaques monkeys who were exposed to the same strain of SARS-CoV-2 twice in a lab.
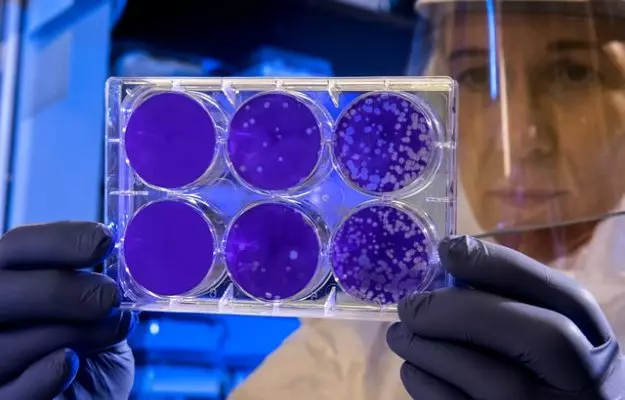
To do this, the scientists injected the virus into these monkeys. During the early stages of recovery, the scientists injected an identical strain of the virus into the monkeys for a second time. Then, the scientists kept a lookout for signs of reinfection, such as the pneumonia-like symptoms associated with COVID-19.
The primates did not present with the symptoms—either through replication of the virus in the body or any other changes associated with the infection—after the second injection.
The study showed that the primates had developed antibodies against the infection and launched an appropriate immune response the second time, indicating that previous exposure to the virus was able to help them avoid the infection soon afterwards.
The scientific community has been divided over the symptoms of COVID-19 returning in patients who have already recovered from the disease, with several cases being recorded in countries around the world. A study published in the preprint server medRxiv looked at antibody responses in patients diagnosed with COVID-19, and found that it was dependent on the severity of the infection in the first place. (Read more: Who is immune to COVID-19)
A study published in The New England Journal of Medicine took antibodies from 34 patients who had recovered from mild COVID-19 and did not require intensive care. The antibodies were analysed twice, once 37 days after the onset of symptoms and again almost three months later, only to find out that the antibody levels had rapidly declined in that time. In fact, they also observed that the antibodies had fallen faster than in the case of SARS, which had broken out in 2002-03.
Experts on the subject have found that antibodies peak in the body between 20 to 30 days after the onset of symptoms, but begin to decline sharply after that, alarming people over the possibility of reinfection. This is a critical topic for epidemiologists and the larger scientific community which has been hard at work to develop vaccines and treatment strategies against the infection.
Read more: The role of T cells in immunity to COVID-19
The possibility of reinfection means vaccines, once developed, may have to be given in multiple doses to control the spread of COVID-19. A study conducted by the Centers for Disease Control and Prevention of South Korea tested 285 patients who had recovered from the infection, and included patients who were showing symptoms of COVID-19 months after being diagnosed for the first time.
However, none of the samples showed enough viral presence to be able to replicate, leading the researchers to believe that the remaining viral particles found in the samples may have been dead viruses.
Not enough evidence about widespread reinfection has been recorded, which has made it difficult to explain the stray cases of people becoming infected with the SARS-CoV-2 virus twice. Infectious disease experts, though, have cited the examples of chickenpox and other viral infections also returning, even though it is well known that antibodies for such diseases do not allow reinfections to reappear.
But the reverse of this is also true. According to the World Health Organization (WHO), there isn't any evidence of people being protected from becoming reinfected either.