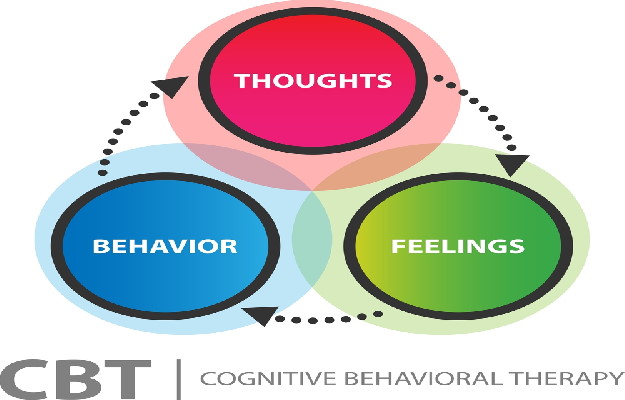
Cognitive behavioural therapy (CBT) is a therapeutic intervention in which a psychologist tries to change extreme and unhelpful thought patterns and behaviours in their patient, and to build problem-solving capabilities and achieve set goals.
At the heart of CBT are three principles:
- Unhelpful or erroneous ways of thinking can lead to or worsen psychological problems. Some types of “thinking errors” that therapists try to address in CBT sessions are:
- All-or-nothing thinking: A tendency to see things in black and white—you’re either perfect at something or you’re terrible, there is no room for being good or even great. According to this worldview, being 90% good at something is like not being successful at it at all.
- Labelling: A tendency to label ourselves and others based on one trait or experience. For example, someone with this distortion might think they are unlovable because someone broke up with them. Or they might think someone else is totally incompetent because they made a mistake.
- Filtering: A tendency to filter out the positive or good news and focus only on the bad things that happen to you can also skew your worldview.
- Should-be error: A tendency to focus on how things should be rather than how they are and what is the best way to deal with them.
- Personalization: A tendency to think that other people are thinking about you or making fun of you or are angry with you when in fact they are most likely busy with their own lives.
- Catastrophizing: A tendency to escalate negative thoughts quickly. People with this thinking error quickly conclude that the worst things will happen to them. If they get bad marks on one paper, they might think they'll fail the class. If they get behind on payments one month, they might think they will go broke.
CBT tries to help people identify and challenge self-deprecating thoughts like “I am unlovable” or “I don’t deserve a promotion”. In their stead, it tries to equip patients with skills and tools to cope with adverse events more rationally.
- Unhelpful behaviours and patterns are partially responsible for psychological problems. An example of this, cited in the Advances in Psychiatric Treatment journal of the Royal College of Psychiatrists, Cambridge, goes something like this: You get invited to a party. You have negative thoughts about it, such as I won’t have anything to say or anyone to talk to and it will be awful. This type of thinking spirals until you feel like you don’t want to go out or socialise at all. This is an unhelpful behaviour pattern that derives from unhelpful thinking.
- CBT is premised on the belief that people with psychological problems can improve their lives by acquiring the skills and tools to cope with unhelpful thoughts and behaviours.
On World Mental Health Day 2020, observed every year on 10 October to raise awareness and improve access to mental health care for everyone, we bring to you this article on what is CBT, what it involves, how it works and who needs CBT.