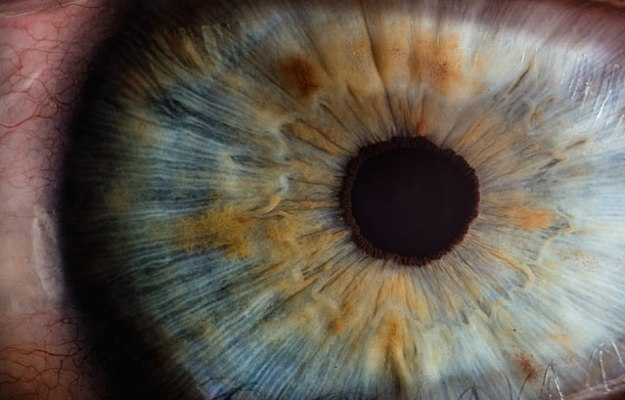
It could be argued that the gift of sight is the most important of all senses. The human eye, with its complex inner workings and intricate design, enables vision.
The eye can be compared to a digital camera. Much like a camera lens, the curved front surface of the eyeball, called the cornea, allows light to be focused. The iris, the coloured part of the eye, functions as a shutter or diaphragm and adjusts the pupil (black circular centre in the coloured iris which is like the aperture) size to regulate the amount of light entering the eye in order to capture the image. Through the pupil, light falls on the crystalline lens of the eye which focuses it more. The light focused by the cornea and the crystalline lens then falls on the retina (innermost layer of the eyeball) which acts as the image sensor and converts the optical image to an electronic signal and the optic nerve takes this signal to the visual cortex in the brain where it’s interpreted.
Eye cancer is an uncommon disease. Primary eye cancer, which begins in the eye, is rarer than secondary eye cancer which spreads from another body part to the eye. While the most common kind of eye cancer in adults is melanoma of the iris, ciliary body and choroid, only five out of a million people get diagnosed with it each year.
Broadly, there are two types of eye cancer. Those that occur in the structures within the eyeball (intraocular) and those that arise in the surrounding supportive tissues like eyelids. Often, eye cancer goes undiagnosed because it is generally painless. Deterioration of eyesight is the usual symptom. External signs may include bulging of the eyeball (proptosis) or lumps in surrounding structures.
Eye cancer is diagnosed using a mix of ophthalmoscopic examination, blood tests and imaging techniques. Definitive treatment could be surgical or radiotherapy. Laser therapy might be added for improved results. Prognosis is generally good unless the cancer has spread to other body parts.

 Doctors for Eye cancer
Doctors for Eye cancer  OTC Medicines for Eye cancer
OTC Medicines for Eye cancer