Summary
Iridectomy is performed to remove a small part of your iris either surgically or by laser (iridotomy). This surgery helps to reduce the increased pressure in the eye caused by certain conditions like melanoma of the iris or angle-closure glaucoma. The procedure is contraindicated in some instances such as if you have had multiple laser iridotomies in the past.
Before the surgery, the doctor will perform some tests, including tonometry and gonioscopy to assess your eye health. A laser iridotomy does not need much preparation; however, if you are undergoing a surgical iridectomy, you will need to fast for about eight hours before the procedure. You can return home on the same day and resume work from the next day of the surgery. To prevent any infections, your doctor will prescribe eye drops and ask you to wear an eye patch. A follow-up generally takes place after two weeks, but if you have any symptoms such as problems in your vision or if your pain worsens, consult your doctor immediately.
- What is iridectomy?
- Why is iridectomy recommended?
- Who can and cannot get iridectomy?
- What preparations are needed before iridectomy?
- How is iridectomy done?
- How to care for yourself after iridectomy?
- What are the possible complications/risks of iridectomy?
- When to follow up with your doctor after an iridectomy?
What is iridectomy?
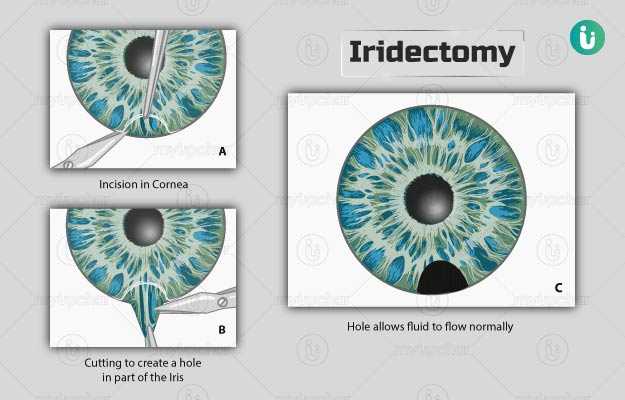
Iridectomy is a surgery in which a portion of the iris (the coloured part in the eye) is removed either surgically or by laser (laser iridotomy). Laser is the method of choice nowadays.
Human eye is divided into two fluid filled parts; the jelly-like vitreous humour in the posterior segment and the watery aqueous humour in the anterior segment. The anterior segment is further divided into anterior and posterior chambers that are separated by the iris. The iris is the coloured part seen in the front of the eye, which is covered by a transparent, dome-like structure, called the cornea. The aqueous humour in the anterior segment of the eye is drained through a meshwork located at the angle of the eye (where the cornea and iris meet). If the angle becomes too narrow, the pressure may build up in the eye (due to improper drainage), causing damage to the optic nerve (situated at the back of the eye). This is known as narrow-angle glaucoma or angle-closure glaucoma.
In iridectomy, a hole or an incision is made in the iris such that the aqueous humour can drain properly and the pressure inside the eye is lowered.
Why is iridectomy recommended?
Iridectomy is recommended in the following conditions:
- Angle-closure glaucoma
- Melanoma of the iris or ciliary body (tumour in the pigment-forming cells in the iris)
A surgical iridectomy may be performed in people before undergoing the following surgeries:
- Surgery for glaucoma
- Implantation of an intraocular lens in the anterior chamber of the eye
A laser iridotomy is recommended in the following conditions:
- Acute angle-closure glaucoma with symptoms like reduced vision, severe eye pain, and headache
- Suspected angle-closure (angle closure is suspected, but no symptoms are seen)
- Intermittent angle closure (sudden rise of intraocular pressure that resolves spontaneously).
Melanomas do not have symptoms in the early stages, but if the symptoms occur, these comprise:
- A dark spot on the conjunctiva or iris
- Sensation of flashing lights
- Change in the shape of the pupil
- Distorted or blurred vision or a blind spot in your peripheral (side) vision.
Who can and cannot get iridectomy?
A doctor may not recommend a laser iridotomy in individuals with:
- Repeated failure or closure of iridotomies
- Extremely narrow angle with iris very near to the corneal endothelium (the inner surface of the cornea)
- A cloudy cornea
The contraindications for surgical iridectomy include:
- Involvement of more than four clock hours (the eye is segmented into 12 sections like a clock) of the iris
- Seeding or diffuse spreading (when a tumour invades a natural body cavity)
What preparations are needed before iridectomy?
Before the surgery, you will need to prepare in the following manner:
- Your doctor may order the following tests:
- Blood tests for blood sugar and haemoglobin, an electrocardiogram (ECG) to check the activity of the heart, and a urine test.
- Tonometry: This measures the pressure in the eye.
- Gonioscopy: This test measures the angle formed between the iris and cornea.
- You do not need any preparation for laser iridotomy. For surgical iridectomy, you will need to fast for about eight hours prior to the surgery.
- You may be asked to stop taking blood thinners like aspirin a few days before the procedure.
- Your doctor may also prescribe you certain use eye drops a few days prior to surgery.
How is iridectomy done?
The procedure for surgical iridectomy is as follows:
- You will be taken to the operating room and asked to lie on the medical table.
- The surgery is performed under local anaesthesia (numbs the area, but you will be awake).
- Your surgeon will place a sterile cloth on your face that will have a hole over your eye.
- With the help of special miniature surgical tools and a small microscope, the surgeon will make an incision in your cornea and cut a part of your iris, generally at the top of the eye to allow drainage.
- The incision on the cornea is self-healing but stitches can be given.
The procedure for laser iridotomy is as follows:
- The doctor will administer eye drops that have the medicine pilocarpine to constrict your pupil.
- You will also be given local anaesthetic drops to numb your eyes.
- You will sit in a special chair, and your head will rest on a support to restrict movement.
- The ophthalmologist (eye doctor) will use a special laser (Nd:YAG laser) to create an opening in your iris to help the aqueous humour drain. This opening is at the extremity of the iris (below the eyelids) and will not cause any harm to your vision.
- Laser iridotomy takes about five minutes.
You can return home on the same day.
How to care for yourself after iridectomy?
Your vision may take about six weeks to get back to normal, and you may need the following care at home:
- Wear an eye patch on the affected eye for several days after the surgery.
- You may also need eye drops to prevent an infection.
- Take aspirin to manage pain.
- You can resume your work and regular activities on the day after surgery.
- You should not indulge in any strenuous activities for three weeks.
- If the iridectomy was performed to reduce intraocular (eye) pressure, you might still need some medication to help control the pressure.
- If the iridectomy was performed for melanoma, you should avoid exposure to any source of ultraviolet light, including sunlight.
The surgical iridectomy or laser iridotomy helps in lowering the eye pressure and removing the tumour of the iris.
When to see the doctor?
See the doctor immediately if you notice any of the following symptoms:
- Pain or discomfort
- Vision not restored to normal
- Worsening of the pain or vision
What are the possible complications/risks of iridectomy?
The common risks of both laser iridotomy and iridectomy include:
- Bleeding
- Failure to reduce pressure in the eye due to closure of the iridectomy
Specific complications related to laser iridotomy include:
- Temporary increase in the eye pressure
- Inflammation of the eye
- Scarring at the point of contact of the laser beam
Some complications specific to iridectomy are as follows:
- Risk of cataract formation and infections
- Scarring at the surgery site
Complications that may occur in an iridectomy for melanoma of the iris are:
- Cataract formation
- Glaucoma due to new blood vessel formation near the angle
- Recurrence of the tumour
When to follow up with your doctor after an iridectomy?
Your follow-up appointment will be scheduled for two weeks after the surgery.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- Schwenn O, Sell F, Pfeiffer N, Grehn F. Prophylactic Nd:YAG-laser iridotomy versus surgical iridectomy: a randomized, prospective study. Ger J Ophthalmol. 1995;4(6):374-379. PMID: 8751104.
- Shields CL, Shields JA, Materin M, Gershenbaum E, Singh AD, Smith A. Iris melanoma: risk factors for metastasis in 169 consecutive patients. Ophthalmology. 2001;108(1):172-178. PMID: 11150284.
- Thomas R, Sekhar GC, Kumar RS. Glaucoma management in developing countries: medical, laser, and surgical options for glaucoma management in countries with limited resources. Curr Opin Ophthalmol. 2004;15(2):127-131. PMID: 15021224.
- Aung T, Chew PT. Review of recent advancements in the understanding of primary angle-closure glaucoma. Curr Opin Ophthalmol. 2002;13(2):89-93. PMID: 11880721.
- Lentschener C, Ghimouz A, Bonnichon P, Parc C, Ozier Y. Acute postoperative glaucoma after nonocular surgery remains a diagnostic challenge. Anesth Analg. 2002;94(4). PMID: 11916819.
- Chang BM, Liebmann JM, Ritch R. Angle closure in younger patients. Trans Am Ophthalmol Soc. 2002; 100: 201-12; discussion 212-4. PMID: 12545694.
- Lee JW, Lee JH, Lee KW. Prognostic factors for the success of laser iridotomy for acute primary angle closure glaucoma. Korean J Ophthalmol. 2009;23(4):286-290. PMID: 20046690.
- American Academy of Ophthalmology [Internet]. California. US; Ocular Melanoma Symptoms
- Columbia University Department of Ophthalmology [Internet]. US; Peripheral Iridectomy
- Singh Arun, Damato Bertil, et al. Clinical ophthalmic oncology. Philadelphia: Elsevier; 2007. Chapter 44, Uveal malignant melanoma: management options – resection techniques; pg 259-266.
- Jackson TL, Thiagarajan M, Murthy R, Snead MP, Wong D, Williamson TH. Pupil block glaucoma in phakic and pseudophakic patients after vitrectomy with silicone oil injection. Am J Ophthalmol. 2001;132(3):414-416. PMID: 11530062.
- Jiménez-Jiménez FJ, Ortí-Pareja M, Zurdo JM. Aggravation of Glaucoma with Fluvoxamine. Ann Pharmacother. 2001;35(12):1565-1566. PMID: 11793621.
- Goldberg, D. E., and Freeman W. R. Uveitic angle closure glaucoma in a patient with inactive cytomegalovirus retinitis and immune recovery uveitis. Ophthalmic Surgery and Lasers. 2002; 33(5): 421-5.
- Kumar, A., Kedar S., Garodia V. K., Singh R. P. Angle Closure Glaucoma Following Pupillary Block in an AphakinPerfluoropropane Gas-Filled Eye. Indian Journal of Ophthalmology. 2002; 50(3): 220-221.
- Jacobi PC, Dietlein TS, Lüke C, Engels B, Krieglstein GK. Primary phacoemulsification and intraocular lens implantation for acute angle-closure glaucoma. Ophthalmology. 2002;109(9):1597-1603. PMID: 12208704.
- Schwartz GP, Schwartz LW. Acute angle closure glaucoma secondary to a choroidal melanoma. CLAO J. 2002;28(2):77-79. PMID: 12054375.
- Wang N, Wu H, Fan Z. Primary angle closure glaucoma in Chinese and Western populations. Chin Med J (Engl). 2002;115(11):1706-1715. PMID: 12609093.
- Shields CL, Materin MA, Shields JA, Gershenbaum E, Singh AD, Smith A. Factors associated with elevated intraocular pressure in eyes with iris melanoma. Br J Ophthalmol. 2001;85(6):666-669. PMID: 11371484.
- Canadian Ophthalmological Society [Internet]. Ontario. Canada; Glaucoma treatment