What is pelvic pain?
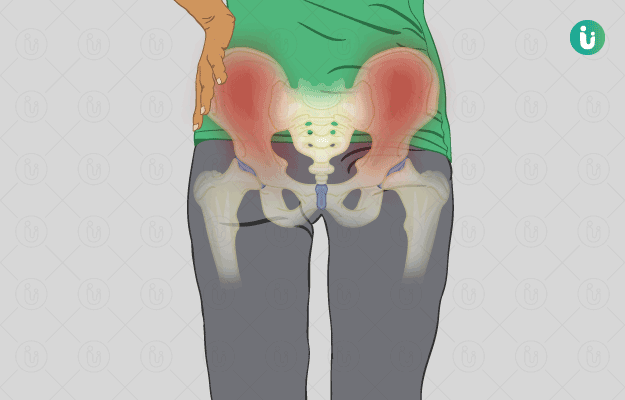
Pelvic pain refers to pain anywhere in the area below the navel due to a disorder of any of the pelvic organs. In females, it may include the disorders of the uterus, ovaries, or the tubes and in males, prostate problems might lead to pelvic pain. Both genders may have pain related to urinary tract infection, pelvic bone and muscle disorders. However, it is most frequently experienced by women.
What are its main signs and symptoms?
The pain is mainly localised to the lower abdominal area. Pain can be dull or sharp that comes and goes (intermittent pain). It can be generalized or spotty (localised) that is limited to specific sites. The cause determines the nature and intensity of pain. The pain may be associated with burning urination, blood in urine, nausea, vomiting, and more.
What are the main causes?
Causes common to both males and females include kidney stones, colitis, spasms of pelvic muscles, urinary tract infections, osteoporosis (reduced bone mineral density after menopause), and sexually transmitted diseases.
Causes in women:
- Ovarian cysts.
- Endometriosis.
- Regular menstrual cramps.
- Infection of the uterus, vagina or cervix.
- Pelvic inflammatory disease.
- Fibroids.
- Tubal pregnancy.
- Cancer in the pelvis.
Causes in men:
- Prostatitis (inflammation of the prostate gland).
- Epididymitis (inflammation of the epididymis).
- Testicular infection.
- Torsion of testes.
Pain localised in the hip area refers to a bone disorder or fracture as the possible cause and requires further evaluation. Right-sided pain can point out an ovarian cyst or pain radiating from an inflamed or swollen appendix (appendicitis).
How is it diagnosed and treated?
Diagnosing the cause of pelvic pain can be challenging, hence, the primary aim of your doctor will always be to elicit a good past and present history. This helps them to understand the exact nature of your pain so as to point out related causes. Your doctor will order certain blood tests and a urine test. Also, he/she might ask you to undergo certain pelvic scans including an ultrasonography and CT scan if needed, to look at the pelvic structures. Treatment depends upon the cause. Painkillers are given to manage acute and severe pain. Muscle relaxants and anti-inflammatory drugs are administered for spasms. In cases of scar formation, surgery is advised.
Self-care includes good posture maintenance and regular exercise. Other therapies include acupressure, vitamin injections and yoga. A regular follow-up is advised for a good and speedy recovery.

 Doctors for Pelvic Pain
Doctors for Pelvic Pain  OTC Medicines for Pelvic Pain
OTC Medicines for Pelvic Pain
 Pelvic Pain articles
Pelvic Pain articles
 Ayurvedic Treatment of Pelvic Pain
Ayurvedic Treatment of Pelvic Pain
 Homeopathic Treatment of Pelvic Pain
Homeopathic Treatment of Pelvic Pain






 Dr. Rachita Narsaria
Dr. Rachita Narsaria

 Dr. Laxmidutta Shukla
Dr. Laxmidutta Shukla