Summary
Glaucoma is a condition in which the optic nerves slowly get damaged. It occurs due to increased pressure within the eye and If not treated on time it can lead to loss of vision. Glaucoma surgery is performed to correct the underlying condition that causes the pressure to rise. The symptoms of glaucoma include loss of vision, especially towards the periphery (side vision), difficulty looking at bright lights, and hazy vision. The surgery is indicated when medications and laser treatments fail. Surgical approaches include trabeculectomy, tube shunt surgery, and the more recent minimally-invasive glaucoma surgeries. However, they carry the risk of complications ranging from short-term to long-term.
- What is glaucoma surgery?
- Why is glaucoma surgery recommended?
- Who can and cannot get glaucoma surgery?
- What preparations are needed before glaucoma surgery?
- How is glaucoma surgery done?
- How to care for yourself after glaucoma surgery?
- What are the possible complications/risks of glaucoma surgery?
- When to follow up with your doctor after a glaucoma surgery?
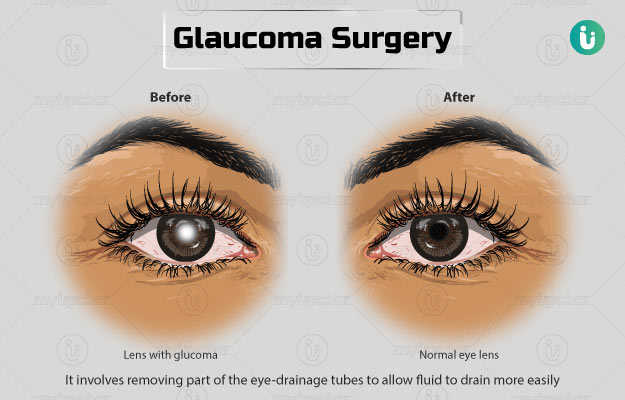
What is glaucoma surgery?
Glaucoma is an eye condition that occurs due to increased intraocular pressure (pressure in the eye). It damages the optic nerve (the nerve that carries the signals to the brain for processing), resulting in blindness. Glaucoma surgery is performed to decrease the intraocular pressure (IOP) within the eye. It may be performed using laser surgery or incisional surgery.
The front portion of the eye, between the iris, pupil, cornea (parts of the eye), and the lens, is filled with a liquid called aqueous humour. A trabecular meshwork at the front of the eye is responsible for draining the aqueous humour. When the meshwork is blocked and the fluid collects, it raises the pressure within the eye. The increase in pressure is not always detrimental, but in some people, it affects the optic nerve. This leads to loss of side (peripheral) vision and consequent blindness if the condition persists for long-term. The normal IOP within the eye is 12 to 21 mmHg.
Surgery is indicated if medications and laser therapy do not improve the condition.
Why is glaucoma surgery recommended?
Your doctor may recommend glaucoma surgery if you have the following conditions:
- Glaucoma that shows signs of disease progression based on perimetry (measuring the visual field) or increase in cup-to-disc ratio (a ratio used to check the progress of glaucoma).
- Ocular hypertension that is unresponsive to medical therapies
- Intraocular pressure that progresses the glaucoma damage, leading to visual disability
- Laser therapy performed earlier was unsuccessful
The symptoms of glaucoma include:
- Headache and eye pain
- Appearance of bright light with halos or rainbow-like hues around them.
- Blurry vision and foggy vision
- Loss of sight
Who can and cannot get glaucoma surgery?
Glaucoma surgery is contraindicated in people who:
- May not develop visual impairment due to glaucoma during their lifetime
- Have a shorter life expectancy due to some other health condition. Even in such a case the surgery may be carried out to reduce pain
- Are not stable enough to have the surgery
- Have considerable scars on the conjunctiva (a thin membrane covering the visible surfaces of the eye and under the eyelid)
- Have phakia or pseudophakia (when a person has no lens in the eye or an artificial lens implant from cataract surgery, respectively)
- Have a corneal condition that requires transplantation later
- Have developed a cataract that will need to be removed in the future
What preparations are needed before glaucoma surgery?
The following preparations are needed before a glaucoma surgery:
- You will have to sign a consent form, giving your approval for the procedure.
- Your doctor will take your medical history and perform a physical examination to check how fit you are for the procedure.
- Eye tests will be performed including those for visual acuity, level of IOP, inflammation or infection in the eye, scarring of the conjunctiva, nerve damage or loss in visual field due to glaucoma, and cataract.
- Inform your doctor about all the medications you take.
- Discuss with your doctor if you have any allergies to medications.
- Do not eat anything the morning of the procedure.
- Inform your doctor if you take anticoagulants like warfarin, aspirin, or supplements containing vitamin E. They may need to be stopped before the surgery.
How is glaucoma surgery done?
The surgery takes place in the operation theatre. Before the surgery:
- The doctor will place a needle in your vein to give you sedatives or any medicines if required during surgery.
- He/she will sterilise the region around the affected eye and cover your face with drapes such that only the eye region is visible.
- You will then be given anaesthetic intravenously. This will help you relax.
- The surgeon will give an injection around your eye to numb the area. The procedure is performed under local (the surgical area is made numb) or general (person is made to fall asleep) anaesthesia.
- You will be asked to keep your head still and lie down flat for the duration of the surgery.
The main types of glaucoma surgeries and their procedures are as follows:
Trabeculectomy
The aim of this surgery is to allow the fluids from within the eye to come out through its walls and under the tissue that covers the eye (conjunctiva), from where they can be absorbed.
- The doctor will use a binocular microscope to look at your eye during the surgery.
- He/she will make a cut to your conjunctiva and fold it back. Next, a cut will be made to your sclera (white part of the eye) and a flap will be created. This flap will be folded backwards, and a few bits of the scleral tissue will be removed to create a cavity within the front compartment of the eye.
- The surgeon will also remove a part of your iris from under the cavity.
- Then, he/she will stretch the flap over the cavity and stitch it using nylon sutures. The sutures act as a valve to control the flow of the aqueous humour and prevent it from leaking out entirely.
- Finally, the surgeon will stitch your conjunctiva to its original position so it covers the sclera. The conjunctiva begins absorbing the fluid that comes out.
- The sutures may be loosened after the surgery to make adjustments in the eye pressure. Therefore, releasable stitches are used.
- The surgeon will cover your eye with an eye pad or shield.
In order to keep the flap functioning like a valve and prevent it from healing itself, anti-healing medication like mitomycin-C or 5-fluorouracil will be used in the eye during the surgery.
On an average, this procedure takes an hour to complete.
Tube-shunt surgery (implant surgery)
Tube-shunt surgery has the same purpose as of trabeculectomy but is carried out in cases where a scar is formed in the surgical area from an earlier surgery. This surgery is preferred in cases of eye inflammation, secondary glaucoma and in some children with glaucoma.
- The surgeon will make an incision and insert a tiny flexible plastic tube with a flat base into the front chamber of your eye. The tube will be extended to the back of your eye, where its flat base is sewn to the sclera of the eye.
- This tube will collect the aqueous fluid. This fluid then gets absorbed into the cavity created near the plastic base.
- In order to prevent the IOP from dropping too low shortly after surgery, the surgeon will stitch the opening of the tube. The stitches will dissolve on their own in about five weeks of surgery.
- This procedure takes around one to two hours to get complete.
Laser ciliodestruction
Laser treatment helps reduce the quantity of aqueous humour released by the ciliary body (the circular-shaped structure that extends from the iris, the coloured portion of the eye) by burning the ciliary structures.
- In this procedure, the surgeon will treat more than half the ciliary body structure of your eye with a laser to lower the fluid generated to a manageable level, but not entirely stop it.
- The surgeon may focus the laser beam in your eye using a special probe. The probe will pass the beam (from outside your eye) through the surface of your eye along a fiber optic cable. Alternatively, a laser beam may be delivered by inserting the probe directly in the front of your eye.
- The approach from the outside of the eye is followed when trabeculectomy and tube shunting have failed.
Minimally invasive glaucoma surgeries:
- Trabectome: The procedure improves the release of aqueous fluid and reduces pressure by taking out a fine layer of the trabecular tissue.
- Canaloplasty and gonioscopy-assisted transluminal trabeculectomy (GATT): These work by opening up the drainage canals through which the fluid leaves the eye.
- iStent: This surgery introduces small metal tubes in the trabecular meshwork of the eye to improve drainage.
You will be allowed to go home on the same day. The next day, your eye will be assessed to ensure that the fluid drains appropriately and the IOP is lowered. The eye pad should be kept in place for a day after surgery.
How to care for yourself after glaucoma surgery?
You should take the following care at home after surgery:
- It is normal to experience blurred vision, soreness, grainy feeling within the eye, watering and irritation of the eye after the surgery. These will improve with time.
- Make sure to keep your face clean, and do not touch your eye. While bathing, care should be taken to avoid bending forward.
- Antibiotic eye drops should be used in the eye every six hours, five times a day, for nearly 90 days. Clean your hands before administering the drops.
- Anti-inflammatory eye drops should be used every two hours initially and then slowly reduced to five to six times a day. This helps keep the cavity open. It should be continued for 60 to 90 days.
- If you suffer from eye pain, non-steroidal anti-inflammatory medications can help.
- Protect your eye from sunlight, and use sunglasses with UVB filters when outdoors.
- For the first six weeks, activities with forward bending, swimming, running, and even sex should be avoided.
- Avoid using eye make-up for a week.
- Resume work only after your doctor permits, especially if your job requires hard labour.
- Avoid driving until your eyesight stabilises.
- Do not sleep on the side of the surgery for a week.
Benefits of glaucoma surgery:
- Helps reduce IOP
- Reduces the risk of loss of vision
When to see the doctor?
You should visit or call a doctor if you experience the following:
- Increased reddening of the eye and a sticky discharge on the eyelids
- Increased pain
- A web-like pattern in your vision
- Declining vision
- Flashing lights
What are the possible complications/risks of glaucoma surgery?
Some possible complications related to trabeculectomy include:
- Problems due to low pressure:
- Variable or blurred vision
- Hypotony maculopathy
- Discomfort in the surgical area
- Bleeding within the eye
- Infection in the early days or later of surgery; chances of developing late infections (in tube shunt surgery)
- Swelling in the macula and central vision area that affects reading (in laser ciliodestruction)
- Retinal detachment
- Changes in refraction, development of cataract, and progressive vision loss are some long-term risks
When to follow up with your doctor after a glaucoma surgery?
A follow-up visit will be scheduled each week for the initial few weeks, and your stitches will be removed within the first two weeks.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- Glaucoma Research Foundation [Internet]. California. US; Glaucoma Surgery
- BrightFocus Foundation [Internet]. Maryland. US; Glaucoma Surgery Series: The Risks and Benefits of Glaucoma Surgery
- National Eye Institute [Internet]. Bethesda (MD). National Institute of Health: U.S. Department of Health and Human Services; Glaucoma Surgery
- Freitas ML. Adult glaucoma surgery. Jaypee Brothers Medical Publishers; 2013. Chapter 4, deep sclerectomy; p. 24.
- American Academy of Ophthalmology [internet]. California. US; Trabeculectomy
- Johns Hopkins Medicine [Internet]. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System; Glaucoma: What Every Patient Should Know
- Irish College of Ophthalmologists [Internet]. Ireland. UK; Glaucoma Filtration Trabeculectomy Surgery
- Kyari F, Abdull MM. The basics of good postoperative care after glaucoma surgery. Community Eye Health. 2016;29(94):29–31. PMID: 27833261
- Norfolk and Norwich University Hospitals: NHS Foundation Trust [Internet]. National Health Service. UK; Glaucoma surgery
- Tezel G, Kolker AE, Kass MA, Wax MB. Late Removal of Releasable Sutures After Trabeculectomy or Combined Trabeculectomy With Cataract Extraction Supplemented With Antifibrotics. J Glaucoma. 1998 Apr;7(2):75-81. PMID: 9559491.