Summary
Vagotomy is a surgical procedure that involves cutting the vagus nerve - the nerve that controls the secretion of stomach acid. The procedure is done for the management of peptic ulcers in patients who present with symptoms such as nausea, vomiting, weight loss, loss of appetite, black or bloody stools, or pain and burning sensation in the stomach, that cannot be relieved with any medical treatment. You will need to fast from midnight before the day of the surgery. Tell your doctor before the surgery if you have an allergy, if you smoke or are pregnant. After the surgery, you will need a follow-up appointment to check your health.
- What is vagotomy?
- Why is the surgery recommended?
- Who can and cannot get vagotomy?
- What preparations are needed before vagotomy?
- How is vagotomy done?
- How to care for yourself after vagotomy?
- What are the possible complications/risks of vagotomy?
- When to follow up with your doctor after a vagotomy?
What is vagotomy?
Vagotomy is a surgery in which the vagus nerve (the nerve in the stomach that controls the emptying of the stomach and the production of stomach acid) is cut to reduce the secretion of stomach acid. The vagus nerve is responsible for the production of one of the chemicals in the body that stimulates the production of gastric acid, the acid in the stomach.
Excessive production of gastric acid can lead to the formation of painful sores called peptic ulcers in the lining of the stomach and duodenum (first part of the small intestine). In some cases, the ulcers may also develop at the lower end of the oesophagus.
The vagus nerve is made of the following branches: The anterior trunk supplying to organs such as the liver and gallbladder; the posterior trunk that sends branches to the solar plexus (a major junction for nerves supplying to the upper abdomen); and some smaller nerve branches that include branches of the anterior and posterior trunks.
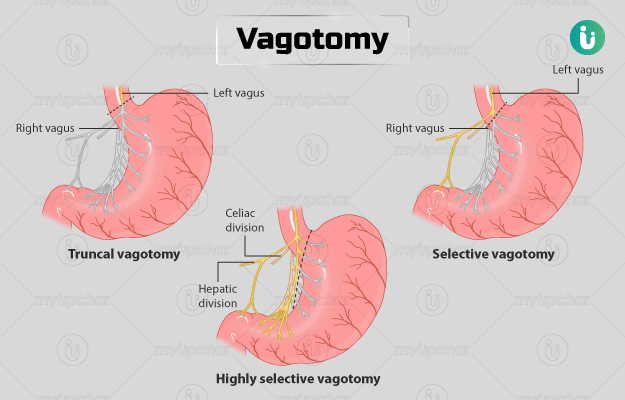
Vagotomy procedures are of three types: truncal, selective, and highly selective vagotomy. The type of vagotomy performed depends upon the type, location, and complications of the peptic ulcer.
Advanced medications developed for peptic ulcer disease have made the vagotomy procedure less common. However, vagotomy is usually indicated in those with a complicated peptic ulcer that has not responded to any other medical treatment.
Why is the surgery recommended?
This surgery is recommended if you have any of the following symptoms of peptic ulcer:
- Pain and burning in the stomach between the breastbone and navel. It usually occurs on an empty stomach or 2 to 4 hours after meals. It may last from a few minutes to hours and is the most common symptom.
- Nausea and vomiting
- Early satiety (feeling full after eating a small amount of food)
- Black or bloody stools
- Reduced appetite or loss of appetite
- Weight loss
- Vomiting blood
Are you also troubled by obesity and are not able to lose weight even after a lot of efforts, then start using myUpchar Ayurveda Medarodh Weight Control Tablet today and control your weight.
Who can and cannot get vagotomy?
The surgery may be recommended if a person is not responding to medications and develops complications related to peptic ulcer such as:
- Bleeding ulcer in the stomach or duodenum
- Perforation (hole) in the lining of the stomach
- Gastric outlet obstruction (the end portion of the stomach that extends into the duodenum shows a blockage that causes improper emptying of the stomach), a rare but severe complication
- Peritonitis: Inflammation of the peritoneum, the tissue lining that covers the organs inside the abdomen and lines the abdominal cavity.
- Recurrence of peptic ulcer after an earlier vagotomy
Vagotomy is contraindicated in the following conditions:
- Severe generalised peritonitis
- Intra-abdominal abscess (inflammation and pus formation within the tissue of the abdomen)
- Pre-operative shock (a life-threatening condition in which the body does not get enough blood circulation)
- Delay of more than 24 hours in the diagnosis and surgery
- Major coexisting medical conditions that may not safely allow for increasing the operation time if needed
What preparations are needed before vagotomy?
You will need the following preparations before the surgery:
-
Diagnostic tests: Your doctor will take a full medical history and conduct a complete physical exam to assess your health. Along with the physical exam, the doctor will ask you to get pre-operative investigations and diagnostic tests done such as:
- Complete blood count
- Kidney and liver tests
- Blood glucose test
- A chest X-ray may be taken before surgery to ensure that your lungs are healthy
- An electrocardiogram (ECG) to check your heart
- Fasting: You will need to fast starting from midnight of the day before surgery until you are fit to eat or drink after the surgery.
- Medicines: You should inform your healthcare practitioner if you take any prescribed, non-prescribed or herbal medicines.
- Tell your doctor if you:
- Are allergic to anything
- Have sleep apnoea
- Have implanted devices in your body
- Smoke
How is vagotomy done?
This surgery is performed in the following manner:
- You will be taken to the operating room.
- Antibiotics will be administered to you 30 minutes before starting the procedure.
- A healthcare practitioner will shave the hair around your abdomen and clean the area to prepare it for surgery.
- You will be asked to lie in supine (lying face upwards) position on the medical table, and an anesthesiologist will give you general anaesthesia.
- A Foley catheter (a tube inserted into your bladder through the urethra to drain out urine) will be placed in.
- Now, the surgeon will make an incision from above your umbilicus (the navel) up to the lower limit of your chest.
- He/she will open your abdomen and inspect it for the presence of the nerve and ulcers.
Truncal vagotomy:
- After the surgeon identifies the nerve, he/she will immobilise and clip it near the junction of your oesophagus and stomach, where the nerve splits into its branches.
- The surgeon will excise up to 2cm of the vagus nerve segment between the clips.
- If there is a peptic ulcer in the stomach, the surgeon may also resect a part of your stomach.
Selective vagotomy:
-
The surgeon will cut the branches of the vagus nerve from near the organs that they supply so that the effect on the other organs (where they supply) is reduced.
Highly selective vagotomy:
-
Only that part of the nerve that affects the stomach directly will be cut. This helps to save other functions of this nerve. It is usually performed along with truncal vagotomy.
After the surgery, the surgeon will close your abdominal wall, and stitch up the overlying skin.
You will have to stay in the hospital for a week. The medical team will monitor your recovery and drain the excess acid secreted by the stomach during this time.
How to care for yourself after vagotomy?
You should take the following care at home after a vagotomy:
Wound care:
- Keep the original dressing in place for at least two days, unless advised by the doctor or unless there is oozing from the wound site.
- Keep the dressing dry. If the dressing gets wet due to any liquid or blood, it should be changed. Before changing the dressing:
- Wash your hands with soap and water.
- Take off the used dressing carefully.
- Avoid touching the wound or the inside of the new dressing to prevent contamination.
- Your stitches will be removed after a week if the surgeon has used non-dissolvable stitches.
Eating and drinking:
- Your doctor may advise a liquid diet until your stomach is able to adapt.
- You should not take spicy food or food that increases acidity. Also, avoid a high carbohydrate diet.
Bathing and showering:
- It is safe to take a bath after coming home unless advised by the doctor.
- Avoiding soaking in the shower for a longer duration, and ensure to pat the wound dry afterwards.
Exercise:
Avoid lifting heavy weights or pulling or pushing for the initial eight weeks after surgery or until the wound has healed completely. A gradual increase in the extent of physical activity, such as going for short walks and gradually increasing the distance is advisable.
Read more: Benefits of walking
When to see the doctor?
Visit or call your doctor if you develop a high fever and wound infection. In the case of wound infection, it may:
- Appear red and swollen
- Become more painful
- Have an unpleasant smell
- Leak blood-like liquid, blood, or pus
What are the possible complications/risks of vagotomy?
Immediate complications associated with vagotomy include injury and bleeding in the oesophagus or the stomach or death. Other complications include:
- Delayed gastric emptying (there is a delay in the passage of solid food from the stomach)
- Infections
- Bleeding
- Diarrhoea
- Recurrence of ulcer
- Post-vagotomy hypergastrinemia (a condition caused by a decrease in acid output after the surgery)
- Dumping syndrome (rapid emptying of the stomach into the intestine, causing symptoms like nausea, vomiting, abdominal cramps and diarrhoea)
When to follow up with your doctor after a vagotomy?
You will need to visit your doctor after three months of the surgery (or earlier if the doctor suggests so) to get your health checked.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- National Institute of Diabetes and Digestive and Kidney Diseases [internet]: US Department of Health and Human Services; Symptoms & Causes of Dumping Syndrome
- Seeras K, Qasawa RN, Prakash S. Truncal Vagotomy. [Updated 2020 Feb 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Johns Hopkins Medicine [Internet]. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System; Peptic Ulcer Disease: Introduction
- Ramakrishnan K, Salinas RC. Peptic ulcer disease. Am Fam Physician. 2007 Oct 1;76(7):1005–12. PMID: 17956071.
- Koop AH, Palmer WC, Stancampiano FF. Gastric outlet obstruction: A red flag, potentially manageable. Cleve Clin J Med. 2019;86(5):345-353. PMID: 31066665.
- Levett DZ, Edwards M, Grocott M, Mythen M. Preparing the patient for surgery to improve outcomes. Best Pract Res Clin Anaesthesiol. 2016;30(2):145-157. PMID: 27396803.
- Sandberg WS, Dmochowski R, Beochamp RD. Safety in the surgical environment. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 9
- Smith SF, Duell DJ, Martin BC, Aebersold M, Gonzalez L. Perioperative care. In: Smith SF, Duell DJ, Martin BC, Gonzalez L, Aebersold M, eds. Clinical Nursing Skills: Basic to Advanced Skills. 9th ed. New York, NY: Pearson; 2016:chap 26
- Hospital for Special Surgery [internet]. New York. US; Anesthesia Frequently Asked Questions
- Herrington Jr J L, Mody B. Total duodenal diversion for treatment of reflux esophagitis uncontrolled by repeated antireflux procedures. Ann Surg. 1976 Jun; 183(6): 636–644. PMID: 973751.
- Kuremu RT. Surgical management of peptic ulcer disease. East Afr Med J. 2002;79(9):454-456. PMID: 12625684.
- Leeman MF, Skouras C, Paterson-Brown S. The management of perforated gastric ulcers. Int J Surg. 2013;11(4):322-324. PMID: 23454244.
- Liu B, Fang F, Pedersen NL, et al. Vagotomy and Parkinson disease: A Swedish register-based matched-cohort study. Neurology. 2017;88(21):1996-2002. PMID: 28446653.
- Pappas TN, et al. (2010). Surgery for peptic ulcer disease in GI/Liver secrets. 4th ed. Philadelphia, PA: Mosby/Elsevier
- University of Rochester Medical Center [Internet]. Rochester (NY): University of Rochester Medical Center; Good Results for Less Invasive Obesity Surgery In Small Study
- Stanford Health Care [internet]. Stanford Medicine. Stanford Medical Center. Stanford University. US; General Surgery
- Rabben Hanne-Line, et al. Vagotomy and Gastric Tumorigenesis. Curr Neuropharmacol. 2016 Nov; 14(8): 967–972. PMID: 26791481.
- Saber Aly, Gad Mohammad A, Ellabban Gouda M. Perforated duodenal ulcer in high risk patients: Is percutaneous drainage justified?. North American Journal of Medical Sciences. 2012; 4(1): 35-39.
- Song Nana, et al. Vagotomy attenuates bleomycin-induced pulmonary fibrosis in mice. Scientific Reports. 2015; 5(13419).
- The Hillingdon Hospitals [Internet]. NHS Foundation Trust. National Health Service. UK; Caring for your surgical wound at home
- Toro P. Juan, et al. Efficacy of Laparoscopic Pyloroplasty for the Treatment of Gastroparesis. Journal of American College of Surgeons. 2014; 218(4): 652-660.
- Association of Surgical Technologists [Internet]. US; Vagotomy with Laparaotomy
- Oxford University Hospitals [internet]. NHS Foundation Trust. National Health Service. U.K.; Discharge advice after surgery on the stomach