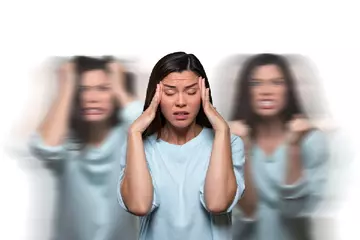
Most women get morning sickness during the early stages of pregnancy. But if the vomiting becomes excessive and persistent, it can cause serious harm to both the mom-to-be and the foetus. The medical term for this condition is hyperemesis gravidarum.
Doctors say that while nausea and vomiting are common in pregnancy, affecting anywhere between 70% and 85% of pregnant women, hyperemesis gravidarum is seen in 0.3% to 2.3% of all pregnancies.
Hyperemesis gravidarum is a serious condition that can cause dehydration, weight loss, electrolyte imbalance and muscle wasting. It requires immediate medical attention, and in most cases, requires hospitalisation to replenish the lost fluids and give nutrition - both fluids and nutrition may be administered intravenously or through a feeding tube.
Though hyperemesis gravidarum can occur anytime before the 20th week of pregnancy, the risk is highest between week nine and week 12 of pregnancy.

 Doctors for Hyperemesis gravidarum during pregnancy
Doctors for Hyperemesis gravidarum during pregnancy