Have you been hearing a lot about gluten lately? It seems like everyone's talking about it, questioning it, or even cutting it out of their diet entirely. But what exactly is this often-debated protein, and how does it really affect your body? Let's dive into the world of gluten to understand what it is, where it's found, and whether it's truly good or bad for you. We'll explore its benefits, potential side effects, and the conditions that might require you to avoid it, helping you make informed decisions about your food choices.
- What Is Gluten?
- Which Foods Are High In Gluten?
- What Are The Benefits Of Gluten?
- What Happens When You Stop Eating Gluten?
- Is It Healthy To Limit Gluten?
- What Are The Side Effects Of Gluten?
- Allergies From Gluten
- Study Around Gluten Associated Medical Problems
- Diseases Form Gluten
- Food To Avoid Gluten Sensitivity And Gluten Tolerance
- Natural Gluten Free Foods
- Benefits Of Gluten Free Foods
- Study About Benefits & Potential Risks of Gluten Free Diet
- FAQ
- Summary
What Is Gluten?
Gluten is a group of proteins naturally found in certain grains, primarily wheat, barley, and rye. It acts as a binding agent, providing elasticity and a chewy texture to doughs. This characteristic is crucial for the structure and rise of many baked goods, contributing significantly to the texture of breads and pastas.
(Read More: What are healthy food and their health benefits)
Which Foods Are High In Gluten?
Gluten is prevalent in a wide array of food products. Major sources include items made from wheat, barley, and rye such as most types of bread, pasta, pizza, cakes, cookies, and breakfast cereals. Beyond these obvious sources, gluten can also be found in less apparent products like soy sauce, some processed meats, certain soups, and many alcoholic beverages, particularly beer. Its properties make it a common additive for binding and texturizing in various processed foods.
What Are The Benefits Of Gluten?
For individuals without specific sensitivities or conditions, gluten is generally considered a safe part of a healthy diet. Whole grains containing gluten, such as whole wheat, are valuable sources of dietary fiber, B vitamins, magnesium, and iron, all vital for maintaining overall health. Some research also indicates that gluten might function as a prebiotic, nourishing beneficial bacteria in the gut, which can support digestive wellness. Therefore, for healthy individuals, a diet incorporating gluten-containing whole grains can offer notable nutritional advantages.
What Happens When You Stop Eating Gluten?
When gluten is removed from the diet, the body's response varies. For individuals with gluten-related disorders or sensitivities, discontinuing gluten intake can lead to a significant alleviation of symptoms like digestive discomfort, fatigue, or headaches. However, for those without an underlying issue, eliminating gluten might lead to a deficiency in essential nutrients commonly found in fortified whole grains. Initial improvements observed after adopting a gluten-free diet may sometimes stem from an overall reduction in processed foods and an increased intake of whole fruits and vegetables, rather than solely from the absence of gluten.
(Read More: Best Home Remedies to Prevent and Treat Food Poisoning)
Is It Healthy To Limit Gluten?
The healthfulness of limiting gluten is highly individualized. For individuals diagnosed with conditions such as celiac disease or specific sensitivities, a gluten-free diet is not only healthy but medically necessary. However, for most healthy individuals, there is no substantial scientific evidence to suggest that avoiding gluten provides significant health benefits. Unduly restricting gluten without careful nutritional planning can sometimes result in inadequate intake of fiber, vitamins, and minerals. Furthermore, many "gluten-free" processed foods might contain higher levels of sugar, unhealthy fats, and calories.
What Are The Side Effects Of Gluten?
The majority of individuals experience no adverse side effects from consuming gluten as part of their regular diet. However, for those with specific sensitivities or conditions, gluten ingestion can trigger various reactions. These can range from mild gastrointestinal symptoms like bloating, gas, and abdominal pain to more systemic issues such as fatigue, headaches, or skin rashes. These side effects are predominantly observed in individuals with an underlying intolerance or diagnosed condition.
(Read More: Vitamin D Sources, Benefits and Side Effects and dosage)
Allergies From Gluten
It is important to distinguish between a gluten intolerance or sensitivity and a true wheat allergy. A wheat allergy involves an immune system reaction to any protein found in wheat, not exclusively gluten, and can be severe.
Symptoms
Reactions typically occur rapidly after ingesting wheat and may include hives, swelling of the face, lips, or throat, respiratory difficulties, nasal congestion, headaches, and in severe cases, anaphylaxis.
Causes
This is an immune-mediated response where the body mistakenly identifies wheat proteins as harmful substances.
How To Cure?
There is currently no cure for a wheat allergy. Management involves strict avoidance of wheat. For severe allergic reactions, emergency epinephrine administration may be required.
Study Around Gluten Associated Medical Problems
The article provides a medical overview and categorization of various diseases and conditions linked to gluten. It emphasizes the importance of understanding the spectrum of gluten-related illnesses for clinicians, including well-known conditions like celiac disease (CD), non-celiac gluten sensitivity (NCGS), wheat or grain allergy, gluten ataxia, and dermatitis herpetiformis (DH). The authors delve into the etiology, presentation, evaluation, and management strategies for these conditions, highlighting the collaborative role of an interprofessional healthcare team in addressing them. The article also touches upon the historical context of gluten research and how perceptions of gluten have evolved over time.
The article underscores that gluten sensitivity is the primary cause of celiac disease, a condition characterized by specific changes in intestinal anatomy that resolve upon strict gluten avoidance. It defines Non-Celiac Gluten Sensitivity (NCGS) as a diagnosis for individuals who experience intestinal or extraintestinal symptoms (or both) after consuming gluten-containing grains, yet do not have celiac disease or a wheat allergy, with their symptoms improving upon gluten withdrawal. Additionally, Dermatitis Herpetiformis (DH) is described as a rare, intensely itchy skin eruption associated with gluten sensitivity and celiac disease, typically presenting as inflammatory papules and vesicles on areas like the forearms, knees, scalp, or buttocks.
The provided article primarily serves as a review and categorization of medical facts concerning gluten-associated conditions. It does not contain details of specific surveys conducted, the results of particular studies, or references to singular studies used to derive its findings. Instead, it synthesizes information from broader medical knowledge and confirmed facts.
While the article discusses the management of gluten-associated conditions and the role of an interprofessional team in evaluation, diagnosis, and management, it does not explicitly outline specific recommendations or implications in separate, distinct sections. Its focus is on reviewing the medical aspects and existing knowledge rather than providing forward-looking guidance or policy implications.
The article concludes by outlining the diverse range of medical problems linked to gluten, from autoimmune disorders like celiac disease to sensitivities and neurological conditions. It serves as a comprehensive resource for healthcare professionals, consolidating current understanding of gluten's impact on human health and the various ways it can manifest as a health concern. The information aims to clarify the distinctions between different gluten-related conditions and guide their clinical approach.
Diseases Form Gluten
For certain individuals, gluten can be a trigger for significant health conditions that extend beyond mere sensitivity. These conditions are specific medical diagnoses.
(Read More: What is Sattvic Food? A Comprehensive Guide to This Pure Diet)
Celiac Disease
This is an autoimmune disorder where consuming gluten causes damage to the small intestine. The immune system attacks the villi, which are crucial for nutrient absorption, leading to malabsorption and a range of symptoms. It is a genetically predisposed condition.
Symptoms
Now, here's where it gets tricky – celiac disease can be quite a chameleon! Its symptoms vary wildly from person to person. You might know someone who feels completely fine but has it, while others experience a wide range of issues. In children, digestive symptoms are often more apparent: think frequent bloating, chronic diarrhea (sometimes described as greasy or foul-smelling), or even surprising constipation, gas, nausea, vomiting, and abdominal pain. Does any of that sound familiar?
But the story doesn't end in the gut. Celiac disease can manifest throughout your entire body. Have you been feeling unusually tired, struggling with depression or anxiety, or just feeling irritable (especially if it's a child)? Joint pain, mouth sores like canker sores, or a persistently dry mouth could also be clues. And then there's dermatitis herpetiformis – a distinct, intensely itchy, blistering skin rash that's often a hallmark of untreated celiac disease in adults. For younger ones, symptoms might include slow growth, delayed puberty, or even issues with tooth enamel. It truly affects more than just your stomach!
Causes
So, what makes this happen? Celiac disease is fascinating because it's an autoimmune condition. This means your body's own immune system, which is supposed to protect you, gets confused. If you have certain genetic predispositions (specifically the HLA-DQ2 and HLA-DQ8 gene variants), and you eat gluten, your immune system mistakenly attacks the delicate lining of your small intestine. Imagine your small intestine covered in tiny, finger-like projections called villi – they're like sponges, soaking up all the good nutrients from your food. When your immune system attacks these villi, they become flattened and damaged, crippling your body's ability to absorb vital vitamins, minerals, and energy. This is why malnutrition can become a serious problem. While genes play a big role, scientists are also looking at environmental triggers, like certain childhood infections, that might "switch on" the disease. And here's another key point: celiac disease can develop at any age, not just in childhood.
Diagnosis
Thinking you might have celiac disease? Getting a proper diagnosis is absolutely crucial. It usually starts with a simple blood test. Your doctor will check for specific antibodies that are often elevated in people with celiac disease. Here's a vital tip: do NOT stop eating gluten before these blood tests! If you cut out gluten, your body might stop producing the antibodies, leading to a false negative result. If your blood tests look suspicious, your doctor will likely refer you to a gastroenterologist. They'll perform an endoscopy – a procedure where a thin, flexible tube with a camera is passed down into your small intestine. This allows them to see the lining directly and take tiny tissue samples (biopsies). These biopsies are then examined under a microscope to confirm if the villi are damaged. Genetic testing can also be a helpful tool; if you don't have the specific genes (HLA-DQ2 and HLA-DQ8), it's highly unlikely you have celiac disease.
Treatment
Now for the good news: the treatment for celiac disease is straightforward, though it requires commitment. The only effective way to manage it is a strict, lifelong adherence to a gluten-free diet. This means completely avoiding all foods and products containing wheat, barley, and rye. Even a tiny crumb of gluten can trigger that immune response and restart the damage to your small intestine.
It might sound daunting, right? But embracing a gluten-free lifestyle allows your small intestine to heal over time, often leading to a dramatic improvement or complete resolution of your symptoms. Imagine feeling well again, with energy and comfort! Being vigilant about reading food labels is key, as gluten can hide in many unexpected places – processed foods, condiments, and even some medications. Working with a registered dietitian who specializes in celiac disease can be incredibly helpful; they can guide you through label reading, identify hidden gluten sources, and ensure you're getting all the nutrients you need from delicious, naturally gluten-free alternatives.
Long-Term Effects (Complications)
What happens if celiac disease isn't diagnosed or treated? If you continue to eat gluten, the ongoing damage to your small intestine can lead to some serious long-term health complications due to chronic malabsorption. Imagine your body constantly starving for essential nutrients.
This can result in:
- Malnutrition and Nutrient Deficiencies: Think iron deficiency (leading to anemia), bone loss (osteopenia and osteoporosis) due to lack of calcium and Vitamin D, or issues with B vitamins.
- Other Autoimmune Disorders: Your risk of developing other autoimmune conditions, like Type 1 diabetes or thyroid problems, can increase.
- Neurological Problems: Headaches, nerve damage (peripheral neuropathy), balance issues, and even seizures are possible in rare cases.
- Reproductive Issues: For women, this might mean irregular periods, difficulty conceiving, or an increased risk of miscarriage.
- Lactose Intolerance: Intestinal damage can sometimes temporarily lead to difficulty digesting dairy.
- Increased Cancer Risk: Though rare, long-standing, untreated celiac disease is associated with a slightly higher risk of certain cancers, particularly of the small bowel.
But here's the empowering part: by strictly adhering to a gluten-free diet, you can significantly reduce the risk of these serious complications. For most, the small intestine heals, symptoms disappear, and they can live full, healthy lives.
(Read More: Olive: Benefits and Side Effects)
Gluten Ataxia
A rare neurological autoimmune disorder, Gluten Ataxia involves the immune system attacking parts of the brain, specifically the cerebellum, in response to gluten. This can impair muscle coordination, balance, speech, and eye movements.
Symptoms
The symptoms of gluten ataxia typically develop gradually and can vary, often mimicking other forms of ataxia, which can make diagnosis challenging. Common symptoms primarily involve issues with movement and coordination. You might notice unsteadiness when walking, often described as a "drunken gait," or difficulty maintaining balance, especially when standing. Fine motor skills can also be affected, making tasks like writing, buttoning clothes, or picking up small objects difficult.
Speech can become slurred or hoarse (dysarthria), and some individuals experience involuntary, rapid eye movements (nystagmus). Other less common symptoms can include muscle weakness, overactive reflexes, muscle stiffness, or even a tingling sensation in the hands and feet (peripheral neuropathy). These symptoms can worsen over time if the condition is left untreated.
Causes
Gluten ataxia is an autoimmune disorder. This means that when a genetically susceptible individual consumes gluten, their immune system produces antibodies not just against gluten but also mistakenly against the Purkinje cells in the cerebellum. These Purkinje cells are crucial for cerebellar function, and their damage or loss leads to the characteristic symptoms of ataxia. Unlike celiac disease, most individuals with gluten ataxia do not experience significant gastrointestinal symptoms, even though some may have underlying intestinal damage without classic celiac disease symptoms. The presence of specific antibodies, such as anti-gliadin antibodies (AGA) and particularly antibodies against transglutaminase 6 (TG6), are often found in individuals with gluten ataxia, indicating this immune-mediated response.
Diagnosis
Diagnosing gluten ataxia can be complex because its symptoms overlap with many other neurological conditions that cause ataxia, and not all doctors are familiar with it. The diagnostic process typically involves:
- Neurological Examination: A thorough evaluation of coordination, balance, speech, reflexes, and eye movements.
- Blood Tests: These are crucial to check for antibodies associated with gluten sensitivity, such as anti-gliadin antibodies (IgA and IgG), anti-tissue transglutaminase (tTG), and specifically anti-transglutaminase 6 (TG6) antibodies, which are considered more specific for gluten ataxia. It's important to continue consuming gluten before these tests for accurate results.
- MRI Scan of the Brain: This imaging test can sometimes show atrophy (shrinkage) in the cerebellum, which is a common finding in gluten ataxia as the disease progresses. It also helps rule out other causes of ataxia like tumors or stroke.
- Gluten-Free Diet Trial: In cases where other causes of ataxia have been ruled out and blood tests suggest gluten sensitivity, a strict gluten-free diet may be recommended. Significant improvement or stabilization of symptoms after several months (sometimes up to a year or two) on this diet strongly supports a diagnosis of gluten ataxia.
Treatment
The primary and most effective treatment for gluten ataxia is a strict, lifelong gluten-free diet. This means completely eliminating all sources of wheat, barley, and rye, including hidden gluten in processed foods and potential cross-contamination. Even trace amounts of gluten can continue to trigger the immune response and lead to further neurological damage.
Adhering to the diet aims to stabilize the disease and prevent further neurological deterioration. While some individuals experience significant improvement in symptoms, others may only see stabilization, especially if cerebellar damage has already occurred. Early diagnosis and strict adherence to the diet are crucial for the best possible outcome. There are no specific medications approved to treat gluten ataxia directly, but supportive therapies like physical therapy, occupational therapy, and speech therapy can help manage symptoms and improve quality of life.
Long-Term Effects (Complications)
If gluten ataxia remains undiagnosed or untreated, the progressive autoimmune attack on the cerebellum can lead to irreversible neurological damage. This can result in permanent problems with balance, coordination, and other motor functions. Cerebellar atrophy, or shrinkage of the cerebellum, is a common finding in untreated cases and signifies lasting damage. The severity of long-term complications depends heavily on the duration of gluten exposure before diagnosis and treatment. Prompt and strict adherence to a gluten-free diet is essential to halt the progression of the disease and preserve neurological function.
(Read More: Diet Plan for Weight Loss)
Dematitis Herpetiformis
Dermatitis Herpetiformis (DH), often called the "celiac rash," is a chronic, intensely itchy, blistering skin condition that is directly linked to gluten sensitivity. It's a key external sign of an underlying autoimmune reaction to gluten, and the vast majority of people with DH also have celiac disease, even if they don't experience the typical digestive symptoms. Despite its name, it has absolutely no connection to the herpes virus.
Symptoms
If you have DH, you'll primarily notice skin problems – specifically, small, clustered bumps and blisters that are incredibly itchy, often with a burning or stinging sensation that appears even before the rash. These lesions typically appear symmetrically (on both sides of the body) on characteristic areas such as the elbows, knees, buttocks, lower back, scalp, and sometimes the face or groin. Because the itching is so intense, these blisters are often scratched off quickly, leaving behind erosions, scabs, or discolored patches of skin that can be lighter or darker than your natural skin tone. While skin issues are primary, some individuals with DH might also experience dental enamel defects or, less commonly, some mild gastrointestinal symptoms like bloating or pain, even if they don't have full-blown celiac disease symptoms.
Causes
Dermatitis Herpetiformis is an autoimmune disorder. Here's how it generally works: when a person with a genetic predisposition (often linked to the same HLA-DQ2 and HLA-DQ8 genes as celiac disease) eats gluten, their immune system produces antibodies against gluten. These antibodies then cross-react with a protein in the skin called epidermal transglutaminase (eTG or TG3). This immune complex (antibodies plus the skin protein) deposits in granular clumps in the superficial layers of the skin, particularly at the tips of the dermal papillae. This deposition triggers an inflammatory response, attracting white blood cells (like neutrophils) to the area, leading to the formation of the characteristic itchy bumps and blisters. So, while it's a skin condition, its root cause is the body's immune reaction to gluten consumed in the diet. DH is very closely linked to celiac disease, indicating a shared autoimmune pathway.
Diagnosis
Diagnosing Dermatitis Herpetiformis usually involves a combination of tests, as its appearance can sometimes be mistaken for other skin conditions like eczema or scabies. The gold standard for diagnosis is a skin biopsy from an area of unaffected skin immediately next to a lesion. This sample is then examined using a technique called direct immunofluorescence, which looks for the characteristic granular deposits of immunoglobulin A (IgA) antibodies in the dermal papillae. This finding is almost always positive in DH.
In addition to the skin biopsy, doctors will often perform blood tests to check for specific antibodies associated with celiac disease, such as anti-tissue transglutaminase (tTG-IgA) and anti-endomysial (EMA) antibodies. If these blood tests are positive and the skin biopsy is characteristic of DH, a small bowel biopsy (which is typically done to confirm celiac disease) is often not strictly necessary, as DH itself is considered a specific cutaneous manifestation of gluten-sensitive enteropathy.
Treatment
The cornerstone of treating Dermatitis Herpetiformis is a strict, lifelong gluten-free diet. Eliminating gluten from your diet is crucial because it addresses the underlying cause of the immune reaction. While the gluten-free diet is the long-term solution, it can take several months to up to two years for the skin rash to completely clear.
To provide immediate relief from the intense itching and blistering, doctors often prescribe oral medications, most commonly dapsone. Dapsone works quickly, usually providing relief within 1 to 3 days, but it requires regular blood monitoring due to potential side effects like anemia. Other medications like sulfapyridine or sulfasalazine may be used if dapsone is not tolerated. Once the gluten-free diet starts to take effect and symptoms are controlled, the medication dose can often be gradually reduced or even stopped. However, continued strict adherence to the gluten-free diet is essential to prevent future flare-ups and reduce the risk of long-term complications.
Long-Term Effects (Complications)
If Dermatitis Herpetiformis is left undiagnosed or untreated, the persistent immune reaction to gluten can lead to several long-term complications, primarily due to the underlying gluten-sensitive enteropathy (celiac disease) that often coexists. These complications include:
- Intestinal Damage and Malabsorption: Even if gastrointestinal symptoms aren't prominent, ongoing gluten exposure can cause damage to the small intestine's villi, leading to nutrient deficiencies (e.g., iron, folate, calcium, vitamin D) and potential long-term issues like anemia or osteoporosis.
- Increased Risk of Other Autoimmune Diseases: Individuals with DH and celiac disease have a higher risk of developing other autoimmune conditions, such as thyroid disorders (e.g., hypothyroidism), Type 1 diabetes, and autoimmune liver diseases.
- Increased Risk of Certain Cancers: Although rare, long-standing, untreated celiac disease (which DH often indicates) is associated with a slightly increased risk of certain cancers, particularly small bowel lymphoma.
Strict and lifelong adherence to a gluten-free diet is paramount for managing DH. It not only clears the skin rash but also helps to heal any intestinal damage, reduces the need for medication, improves nutrient absorption, and significantly lowers the risk of these serious long-term complications, thereby enhancing overall health and quality of life.
(Read More: Shrimp Benefits and Side Effects: What You Need to Know)
Non Celiac Gluten Sensitivity
Individuals with NCGS experience symptoms similar to celiac disease, such as bloating, abdominal pain, and fatigue, after consuming gluten. However, they do not exhibit the intestinal damage or specific autoimmune markers characteristic of celiac disease or a wheat allergy. Diagnosis involves ruling out other conditions and observing symptom improvement on a gluten-free diet.
Symptoms
If you have NCGS, your body might send you various signals after you've eaten gluten. These symptoms can be quite similar to those of celiac disease, affecting both your digestive system and other parts of your body. You might experience bloating, gas, nausea, cramping, or even alternating bouts of diarrhea and constipation.
But it's not just about your gut! Many people with NCGS report symptoms outside the digestive tract. Have you ever felt a persistent headache, brain fog (that cloudy feeling where it's hard to concentrate), or overwhelming fatigue? Joint or bone pain, or even numbness in your arms, legs, or fingers are also commonly reported. Unlike a quick allergic reaction, these symptoms might appear hours or even days after you've consumed gluten. It's a subtle but persistent message from your body.
Causes
The exact cause of Non-Celiac Gluten Sensitivity is still a topic of active research, and it's a bit more complex than a simple direct immune attack like in celiac disease or a typical allergy. While gluten is believed to be a primary trigger, some researchers suggest that other components within gluten-containing grains might also be involved. These include certain carbohydrates known as FODMAPs (Fermentable Oligo-, Di-, Mono-saccharides And Polyols), which are poorly absorbed by some people and can cause digestive symptoms like gas and bloating.
Essentially, in NCGS, your body reacts to gluten (or other components in wheat, barley, and rye) in a way that causes symptoms, but without the intestinal damage or specific autoimmune markers seen in celiac disease, and without the allergic immune response seen in a wheat allergy. It's thought to involve an activation of the innate immune system or other less understood pathways.
Diagnosis
Diagnosing Non-Celiac Gluten Sensitivity can be a bit of a detective mission because there isn't one definitive test for it yet. Instead, it's primarily a "diagnosis of exclusion." This means your doctor will first need to rule out other conditions that cause similar symptoms.
Here's the typical process:
- Rule out Celiac Disease: Your doctor will perform blood tests (like those for anti-tissue transglutaminase antibodies) and potentially an endoscopy with biopsies. Remember, you must be eating gluten for these tests to be accurate!
- Rule out Wheat Allergy: This usually involves blood tests (checking for wheat-specific IgE antibodies) or skin prick tests to see if you have a true allergic reaction to wheat.
- Gluten Elimination and Reintroduction: If celiac disease and wheat allergy are ruled out, your doctor might suggest a trial period (typically 4-6 weeks) on a strict gluten-free diet. If your symptoms significantly improve during this time, you'll then gradually reintroduce gluten back into your diet. If your symptoms return upon reintroduction, especially in a "double-blind, placebo-controlled" challenge (where neither you nor the doctor knows when you're getting gluten), then NCGS is strongly suspected.
It's important to do this under medical supervision to ensure accuracy and avoid unnecessary dietary restrictions.
Treatment
The most effective treatment for Non-Celiac Gluten Sensitivity is to follow a gluten-free diet. By removing gluten from your diet, you can alleviate your symptoms and significantly improve your quality of life. This means avoiding all foods and products containing wheat, barley, and rye.
While a strict gluten-free diet is often recommended, the level of strictness might vary slightly compared to celiac disease, depending on individual symptom severity. Some individuals with NCGS might find that they can tolerate very small amounts of gluten occasionally without severe reactions, though many choose to maintain a strict gluten-free diet for consistent symptom relief. Consulting with a healthcare provider or a registered dietitian is highly recommended to help you navigate this diet, identify hidden gluten sources, and ensure you maintain nutritional balance. Some people with NCGS may also benefit from a low-FODMAP diet, as FODMAPs are found in many gluten-containing grains and can contribute to symptoms.
Long-Term Effects (Complications)
Unlike celiac disease, Non-Celiac Gluten Sensitivity is not typically associated with the same kind of irreversible intestinal damage (like villous atrophy) or severe nutrient malabsorption. This means that, based on current understanding, NCGS does not carry the same increased risk of long-term complications such as malnutrition, osteoporosis, or specific cancers that are seen with untreated celiac disease.
However, the chronic symptoms of NCGS can significantly impact a person's quality of life. Persistent fatigue, brain fog, digestive discomfort, and pain can lead to reduced well-being, anxiety, or depression. While not life-threatening in the same way as celiac disease, managing NCGS through a gluten-free diet can bring immense relief and improve daily functioning, preventing the ongoing distress caused by its symptoms. Continued research is exploring the long-term impact of NCGS on overall health.
(Read More: Soda Water: Refreshing Friend or Fizzy Foe? Benefits)
Food To Avoid Gluten Sensitivity And Gluten Tolerance
A strict gluten-free diet is essential for individuals with diagnosed gluten sensitivity or related diseases. This includes avoiding:
- Wheat: All variants and derivatives, including durum, spelt, khorasan (Kamut), farro, semolina, couscous, and einkorn.
- Barley: Commonly found in malt, malt extract, malt vinegar, and most beers.
- Rye: Used in rye bread and pumpernickel.
- Triticale: A hybrid grain of wheat and rye.
- Oats: While naturally gluten-free, oats are frequently subject to cross-contamination during processing with wheat, barley, or rye. Only certified "gluten-free" oats should be consumed by sensitive individuals.
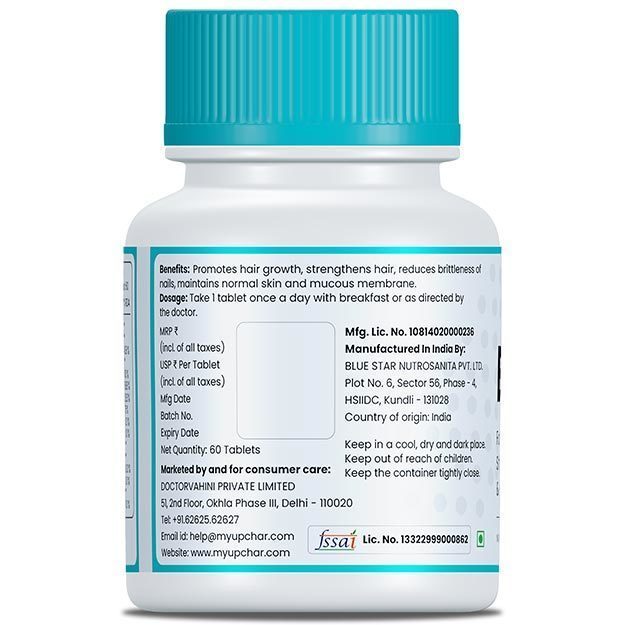
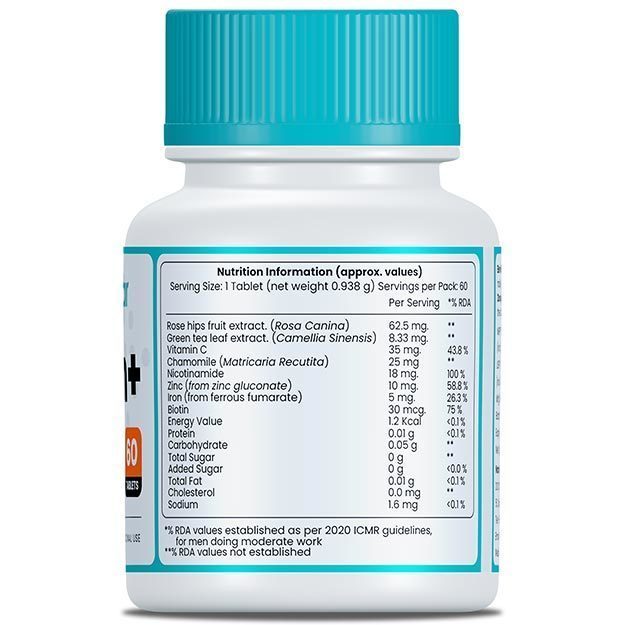
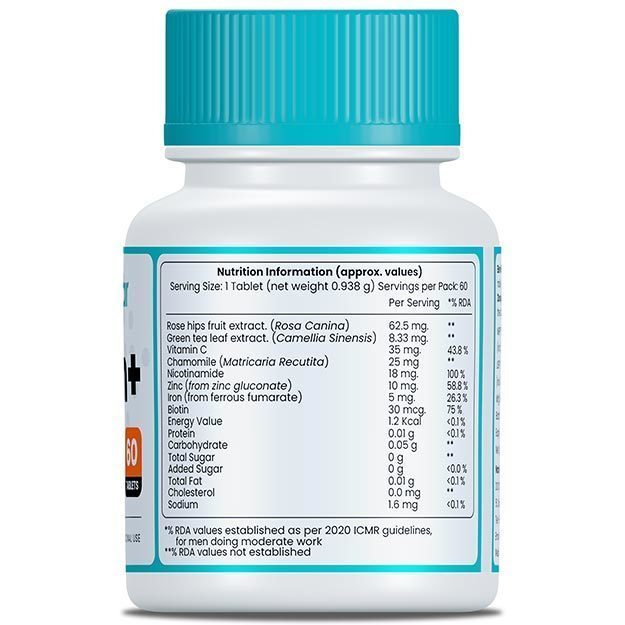
Careful attention to food labels is also necessary, as gluten can be a hidden ingredient in various processed foods like sauces, dressings, processed meats, and certain medications or supplements.
Natural Gluten Free Foods
A wealth of naturally gluten-free foods are available, allowing for a diverse and nutritious diet. These include:
- Fruits and Vegetables: All varieties.
- Meats and Poultry: Fresh, unprocessed cuts of chicken, beef, fish, and other proteins.
- Eggs: A versatile and protein-rich food.
- Dairy: Most natural dairy products such as milk, cheese, and plain yogurt.
- Legumes: Beans, lentils, and chickpeas are excellent sources of fiber and protein.
- Nuts and Seeds: Almonds, walnuts, chia seeds, and flax seeds offer healthy fats and nutrients.
- Naturally Gluten-Free Grains: Rice (including brown, white, and wild varieties), quinoa, corn, certified gluten-free oats, millet, sorghum, amaranth, and buckwheat.
(Read More: Balanced Diet: Chart, Benefits, Importance and Definition)
Benefits Of Gluten Free Foods
For individuals who medically require a gluten-free diet, the benefits are significant and positively impact their health and well-being. These advantages include:
- Relieves digestive symptoms. A gluten-free diet is often taken up by people to treat digestive problems like bloating, gas, diarrhoea or constipation. Studies show that a gluten-free diet can relieve these symptoms. However, it’s important to avoid processed “gluten-free” snacks, as they can quickly add a lot of calories to your diet.
- Reduces joint pain. With celiac disease, comes an increased risk of inflammation. This is why joint pain, especially in the knees, back and wrists is a common symptom of celiac disease. A gluten-free diet will help to prevent this type of joint pain.
- Improves skin. Gluten intolerance can negatively affect your skin. Dermatitis herpetiformis (Duhring's disease), a condition in which the skin blisters, is a manifestation of celiac disease. A gluten-free diet can make the skin more radiant by improving its overall health and while, at the same time, dealing with these problems.
- May boost energy. If you have celiac disease, switching to a gluten-free diet may help boost your energy levels and stop you from feeling tired and sluggish. This tiredness is usually the result of malnutrition due to damage sustained by the gut.
May aid in weight loss. A gluten-free diet eliminates many junk foods that add unnecessary calories to the diet. These foods are often replaced by plenty of indigenous grains and seeds that can be great for weight loss.
(Read More: Mindful Eating: How to Eat Food the Right Way)
Study About Benefits & Potential Risks of Gluten Free Diet
The review comprehensively examines the gluten-free diet (GFD), detailing its historical context, current applications, and nutritional implications. It explores the necessity of the GFD for individuals with celiac disease (CD), wheat allergy, and non-celiac gluten sensitivity (NCGS), while also addressing its increasing adoption by individuals without these conditions. The review discusses the potential benefits and risks associated with the GFD, including its effects on nutrient intake and overall health.
The review highlights that the GFD is the only established treatment for celiac disease, leading to significant improvements in symptoms and intestinal healing. It acknowledges the growing recognition of NCGS as a distinct condition, characterized by symptoms similar to CD but without the same intestinal damage. The article also points out that while the GFD can be beneficial for individuals with these conditions, it's not inherently healthier for the general population and may even lead to nutritional deficiencies if not carefully managed.
The article synthesizes findings from various studies to support its conclusions. It references research indicating that a significant percentage of individuals without diagnosed gluten-related disorders follow a GFD, often driven by perceived health benefits or weight loss goals. The review also cites studies highlighting potential nutritional deficiencies, such as lower fiber, iron, folate, and B vitamin intake, associated with poorly planned GFDs.
The review emphasizes the importance of a well-balanced GFD, particularly for those with celiac disease, to ensure adequate nutrient intake. It suggests that individuals considering a GFD, especially without a medical diagnosis, should consult with a healthcare professional or registered dietitian. The article cautions against the indiscriminate adoption of the GFD, as it may not offer additional health benefits for the general population and could lead to unnecessary dietary restrictions and potential nutrient deficiencies.
"The Gluten-Free Diet: A Comprehensive Review" provides a balanced perspective on the GFD, acknowledging its necessity for certain medical conditions while cautioning against its unnecessary adoption by the general public. It underscores the importance of informed decision-making and professional guidance when considering a GFD, to maximize potential benefits and minimize potential risks.
FAQ
Is Gluten Free Better Than With Gluten?
For most people, a diet that includes whole grains containing gluten is considered healthy and provides important nutrients. A "gluten-free" label does not inherently equate to being "healthier" for everyone; it simply indicates the absence of gluten. While essential for individuals with specific medical conditions, it may be an unnecessary restriction for others.
What Type Of People Can’t Eat Gluten?
Individuals diagnosed with celiac disease, non-celiac gluten sensitivity, wheat allergy, Dermatitis Herpetiformis, or Gluten Ataxia must adhere to a gluten-free diet. A professional medical diagnosis is crucial before making significant dietary changes.
(Read More: Grains: Health Benefits and Side Effects)
Why Is Everyone Avoiding Gluten?
The increased awareness of gluten-free diets stems from a rise in diagnosed gluten-related disorders and a broader wellness trend. Many individuals without a specific diagnosis choose gluten-free diets, often believing it aids in weight management, improves digestion, or enhances overall health. Sometimes, observed benefits may be due to an overall shift towards a healthier, less processed diet rather than solely the elimination of gluten.
Is Gluten Bad For My Skin?
For the majority, gluten does not negatively impact skin health. However, for individuals with Dermatitis Herpetiformis or certain inflammatory skin conditions, gluten can indeed trigger or worsen skin problems. Persistent skin issues linked to gluten consumption should be discussed with a doctor.
Is Gluten Bad For My Gut?
For most individuals, gluten is processed by the gut without adverse effects and may even support gut health by acting as a prebiotic. Conversely, in celiac disease, gluten causes significant damage to the intestinal lining. In non-celiac gluten sensitivity, it can lead to various digestive discomforts. Therefore, gluten is only detrimental to gut health if an individual's gut has a specific adverse reaction to it.
Can I suddenly become Gluten Intolerant?
While the onset of gluten intolerance may seem sudden, it is more common for symptoms to develop gradually over time or for a pre-existing condition to become more pronounced. Bodily systems and immune responses can change throughout life, and factors such as illness, stress, or alterations in gut microbiota can sometimes contribute to the manifestation or worsening of sensitivities. If new or concerning symptoms arise after gluten consumption, consulting a healthcare professional is advisable for proper diagnosis and guidance.
(Read More: Dietary supplements: Benefits and side effects)
Summary
In essence, gluten is a protein found in grains like wheat, barley, and rye, contributing to the texture of many foods. For the majority of people, it is a healthy component of a balanced diet, offering valuable nutrients. However, for individuals with specific autoimmune conditions such as celiac disease, or sensitivities like non-celiac gluten sensitivity, gluten can lead to a range of uncomfortable or serious health issues. The most important takeaway is the importance of individual understanding: if concerns arise regarding gluten consumption, seeking a professional medical diagnosis is vital. This allows for informed dietary choices that support personal health and well-being, whether it involves a gluten-inclusive or gluten-free diet.
Find Dietician in cities
Doctors for Your Complete Guide to Gluten: Foods, Benefits, and Health Considerations

Dt. Vinkaljit Kaur
Dietician
6 Years of Experience

Dt. khushboo fatima
Dietician
11 Years of Experience

Dt. Priti Kumari
Dietician
2 Years of Experience