Summary
Femoral head ostectomy is a surgical procedure wherein the upper portion of the femur (thighbone), which is a part of the hip joint, is removed. The surgery is usually done to treat infections and other complications that occur in individuals following hip transplant surgery. The operation is performed with general anaesthesia or anaesthesia that numbs the lower part of the body. During the surgery, the affected portion of the femur is cut and removed, and the cavity thus formed is replaced with muscles taken from the thigh. Femoral head ostectomy results in shortening of the operated leg. So, individuals who undergo this procedure have a discrepancy in their leg length and have to extensively depend on walking aids.
- What is femoral head ostectomy?
- Why is femoral head ostectomy recommended?
- Who can and cannot get femoral head ostectomy?
- What preparations are needed before femoral head ostectomy?
- How is femoral head ostectomy done?
- How to care for yourself after femoral head ostectomy?
- What are the possible complications/risks of femoral head ostectomy?
- When to follow up with your doctor after a femoral head ostectomy?
What is femoral head ostectomy?
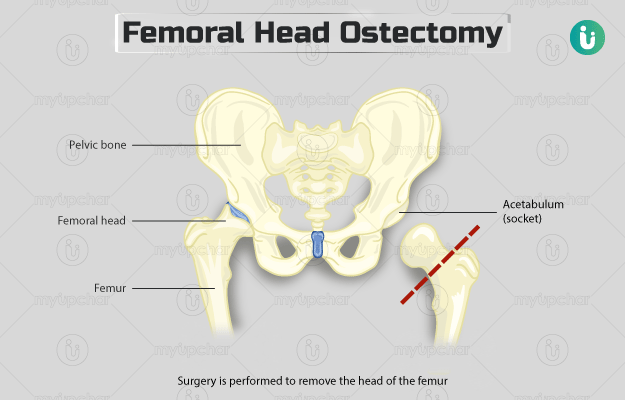
Femoral head ostectomy is a surgery performed to remove the portion of the femur bone that forms the hip joint. The hip joint is a ball and socket joint. The ball part is the top portion of the femur (thighbone), while the socket part is called the acetabulum, a part of the hip bone.
This surgery was first described over 100 years ago in the mid-20th century. It was then used as a life-saving measure for the treatment of tuberculosis-affected hip joint and other hip disorders. However, excision of a part of the femur results in a shortened limb.
Femoral head ostectomy has mostly been replaced by hip replacement surgery but is still performed for very few conditions, including treatment of hip joint infection resulting from an artificial hip implant following the repeated failure of other treatments.
Why is femoral head ostectomy recommended?
This surgery is recommended in individuals who have undergone total hip replacement surgery and have the following conditions after it:
- Peri-prosthetic infection: Infection around the artificial hip implant resulting in symptoms such as pain, swelling, or fever.
- Recurrent dislocation: In this condition, the ball part of the femur keeps on coming out of the socket area.
- Aseptic loosening: The condition results in loosening of the bond between the bone and the artificial hip implant (in the absence of any infection), resulting in pain and disability.
- For the treatment of fracture in the upper part of the femur after other treatment options have failed.
Who can and cannot get femoral head ostectomy?
The surgeon may not perform the surgery in individuals with the following conditions:
- Infection that cannot be treated or controlled with surgery.
- The bone and soft tissue covering the hip joint is not strong enough.
- Unfit for the procedure due to the presence of coexisting medical conditions.
What preparations are needed before femoral head ostectomy?
You will be asked to visit the hospital for a preoperative assessment a few days prior to the surgery. Your surgeon will conduct a few tests, including blood and urine tests, and a pregnancy test. He/she will check your medical history, and ask you:
- If you have any allergies.
- To share a list of all the medicines that you take, including herbs and over-the-counter medications.
- To discontinue blood-thinning medicines such as ibuprofen, aspirin, warfarin, or clopidogrel.
- To quit smoking if you do. This will help reduce the risk of complications associated with the surgery
- To shower and remove nail-polish, make-up, and body piercings before arriving at the hospital on the day of the surgery.
- To tell him/her if you have flu, cold, or fever on the days leading to the surgery. In such a case, your surgery may be postponed.
- Arrange for a friend, family member, or responsible adult to drive you home after discharge from the hospital.
- To fast from the midnight of the night before the surgery. Fasting is recommended to prevent vomiting (a side effect of general anaesthesia) during the surgery.
- To sign an approval or consent form to grant your permission for the surgery.
How is femoral head ostectomy done?
After you arrive at the hospital, the hospital staff will provide you with a hospital gown. They will insert an intravenous line (IV) in your arm or hand to supply essential fluids and medicines during the surgery. You will undergo an X-ray or other imaging procedures before the surgery to allow the surgeon to look at your hip joint and plan the procedure accordingly. This procedure is generally performed using spinal anaesthesia (medicine that numbs the lower part of your body) or general anaesthesia (medicine that makes you unconscious) and is done in the following way:
- You will lie on an operating table either on your chest or side.
- The surgeon will make an incision (cut) on your skin in the side of your thigh.
- He/she will separate and move aside the muscles and tissue beneath your skin to access to the femur bone.
- Then, the surgeon will use special surgical instruments, namely an oscillating saw (a surgical saw used for cutting bones and hard tissues) and an osteotome (a tool used for preparing and cutting bone) to cut the upper section of your femur.
- He/she will grasp the cut portion of your femur with forceps and elevate it to help cut the soft tissues and muscles attached to the bone.
- Next, the surgeon will remove the cut part of your femur from the joint socket and fill the cavity created with muscles from your thigh region.
- He/she will stitch the muscle placed in the cavity to the adjacent muscles and tissues covering the joint and then close the incision using sutures.
After the surgery, the hospital staff will shift you to the recovery room, and another imaging test will be performed to check the success of the surgery. If the surgery was conducted with general anaesthesia, you might feel tired and groggy on waking up afterwards. In addition, you may also experience side effects such as sore throat, dry mouth, and restlessness. These effects disappear within a few hours. You will be put on certain medications, including antibiotics during your hospitalisation post-surgery. Your vital functions will also be continuously monitored. After about three weeks, your stitches will be removed. A physical therapist will visit you after four weeks and help you with range-of-motion exercises and progressive sitting programmes. The surgeon will discharge you from the hospital when you are able to operate a wheelchair independently and move around adequately.
How to care for yourself after femoral head ostectomy?
Your surgeon will provide you with certain instructions to take care of yourself after the surgery. A majority of the individuals do not experience pain after a femoral head ostectomy. However, if you do feel pain, the surgeon may prescribe some medications. Take them as directed.
A physical therapist will help you learn using walking aids as it is a necessary consequence of the surgery.
When to see the doctor?
Contact the surgeon if you experience any of the following signs/symptoms of infection after the surgery:
- Fever
- Chills
- Foul-smelling discharge from the incision
- Pain, redness, and warmth in the operated area
What are the possible complications/risks of femoral head ostectomy?
The surgery impairs the quality of life of the individual due to shortening of the operated leg and causing hip instability, resulting in extensive dependence on walking aids.
Some of the postoperative complications associated with the surgery are:
- Hip infection
- Formation of blood clots in legs
- Opening of the stitches on the wound
- Reaction to anaesthesia
- Cancer in the operated area
- Need for amputation
- Recurrent formation of ulcers in the operated area
When to follow up with your doctor after a femoral head ostectomy?
Before getting discharged from the hospital, your surgeon and physical therapist will provide you with a schedule for follow-up appointments. The follow-up and therapy required after the surgery may vary from person-to-person.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
Doctors for Femoral head ostectomy

Dr. Manoj Kumar S
Orthopedics
8 Years of Experience

Dr. Ankur Saurav
Orthopedics
20 Years of Experience

Dr. Pritish Singh
Orthopedics
12 Years of Experience

Dr. Vikas Patel
Orthopedics
6 Years of Experience
References
- University of Rochester Medical Center [Internet]. University of Rochester. New York. US; Hip Problems
- Maguire N, Robertson B, Henman P. Girdlestone procedure for avascular necrosis of the hip in an intravenous drug user. J Surg Case Rep. 2014 Aug 8;2014(8):rju039. PMID: 25107940.
- Somani AM, Rabari YB, Mulay SD, Saji MA, Ghorpade K, Singh A. Girdlestone resection arthroplasty – a limb salvage procedure after failed hip surgery in a rural setup. Int J Orthopaed Sci. 2017;3(2):449–451.
- Sharma H, De Leeuw J, Rowley DI. Girdlestone resection arthroplasty following failed surgical procedures. Int Orthop. 2005 Apr;29(2):92–95. PMID: 15703933.
- Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014 Apr;27(2):302–345. PMID: 24696437.
- Orthoinfo [internet]. American Academy of Orthopaedic Surgeons. Rosemont. IL. US; Total Hip Replacement.
- Cedars Senai [Internet]. California. US; Aseptic Loosening
- Vincenten CM, Gosens T, van Susante JC, Somford MP. The Girdlestone situation: a historical essay. J Bone Jt Infect. 2019 Sep;4(5):203–208. PMID: 31700767.
- National Health Service [Internet]. UK; Having an operation (surgery)
- Hernandez A, Sherwood ER. Anesthesiology principles, pain management, and conscious sedation. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 14.
- Miller RD, ed. Miller’s Anesthesia. 8th ed. Philadelphia, PA: Elsevier Saunders; 2015
- Rubayi S, Gabbay J, Kruger E, Ruhge K. The modified Girdlestone procedure with muscle flap for management of pressure ulcers and heterotopic ossification of the hip region in spinal injury patients: a 15-year review with long-term follow-up. Ann Plast Surg. 2016 Dec;77(6):645–652. PMID: 26808772.
- Sharma H, Dreghorn CR, Gardner ER. Girdlestone resection arthroplasty of the hip: current perspectives. Curr Orthop. 2005 Oct 1;19(5):385–392.
- Basu I, Howes M, Jowett B, Levack B. Girdlestones excision arthroplasty: current update. Int J Surg. 2011;9(4):310–313. PMID: 21315188.
- Moucha CS. Surgical site infection prevention. In: Browner BD, Jupiter JB, Krettek C, Anderson PA, eds. Skeletal Trauma: Basic Science, Management, and Reconstruction. 5th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 22.