Summary
The surgical procedure of osteotomy involves trimming and fixation of a bone to relieve osteoarthritis pain. The surgery is recommended when pain management measures such as medicines, weight loss, and exercises have failed to ease the discomfort. Before the surgery, you will be asked to get imaging scans of your joint for a careful evaluation of your bones and planning of the procedure. Your doctor will ask you about your lifestyle habits, medical history and history of allergies.
The surgery can take up to one to two hours for completion. Post-surgery as per your condition, you will be allowed to go home the same day or may have to stay in the hospital for up to two days. A nurse/medical team will teach you the use of crutches to reduce weight on your joints. Your doctor may also suggest rehabilitation exercises to strengthen your recovery after the surgery.
- What is osteotomy?
- Why is osteotomy recommended?
- Who can and cannot get an osteotomy?
- What preparations are needed before an osteotomy?
- How is osteotomy done?
- How to care for yourself after osteotomy?
- What are the possible complications/risks of osteotomy?
- When to follow up with your doctor after an osteotomy?
What is osteotomy?
Osteotomy is a surgical approach that involves the removal of some part of a bone in a joint. Surgeons opt for this procedure to reduce osteoarthritis pain.
Osteoarthritis is the “wear and tear” of the cushioning tissue at the juncture of bones in joints (cartilage). The condition ultimately leads to rubbing of the bones on each other, resulting in severe pain and changes in the joint. If you have osteoarthritis, your doctor may initially suggest non-operative measures such as painkiller medicines, exercises, weight loss, and physiotherapy to manage your pain. However, if these measures are ineffective, then he/she may opt for surgeries such as joint replacement or osteotomy based on your condition.
Osteotomy is usually performed for osteoarthritis in the knee. In this case, the bone above the knee (femur) or the bone below the knee (tibia) will be operated on. The surgery will minimise your pain and improve knee movement.
Troubled by obesity? Failed to lose weight? Now control weight easily by myUpchar Ayurveda Medarodha Weight Control Tablet. Get started today and take steps towards a healthy life."
Why is osteotomy recommended?
Your healthcare practitioner will perform this surgery if you have osteoarthritis in your joints or if your joint function has been affected and you have symptoms such as the following:
- Pain
- Stiffness in joints
- Muscle weakness
- Creaking sounds in joints
- Tenderness in joints
- Unusual or swollen appearance of joints
- Increased intensity of pain and stiffness while moving your joint after a long time
- Reduced muscle mass
- Extreme pain in the knee joints while walking or climbing staircases
- Discrepancy in the length of the leg
- Disturbance in gait
Who can and cannot get an osteotomy?
Your surgeon may not perform osteotomy of the femur if you have the following conditions:
- Inflammatory arthritis (painful inflammation or swelling in the joints)
- Infection
- Osteonecrosis (a decrease in blood flow that causes cell death)
- Restricted hip movement
- Advanced stage of osteoarthritis
A tibial osteotomy is not done if you:
- Are more than 65 years of age
- Have severe medial compartment osteoarthritis (arthritis in the medial compartment of the knee)
- Have tricompartmental osteoarthritis (a type of arthritis that affects all parts of the knee)
What preparations are needed before an osteotomy?
Before performing this surgery, you will need to prepare yourself in the following ways:
- The healthcare practitioner will ask you to undergo various tests, such as imaging scans of your knee.
- Share the details of your current and previous medicines including prescribed or non-prescribed medicines or herbal medicines and supplements with your doctor. Also tell him/her if you have any allergies.
- You may need to stop the use of blood-thinning medicines such as aspirin, warfarin or ibuprofen before the surgery.
- Your doctor may ask you to fast from midnight before the surgery until you are deemed fit to eat or drink after the procedure.
- You should stop smoking and drinking before the surgery (or quit altogether) for a speedy recovery afterwards.
- Arrange for someone to drive you home after the surgery.
- You will be asked to sign a consent form, giving your permission for the surgery.
How is osteotomy done?
Osteotomy of the knee will be done in the following way:
- An anaesthetist (a specialist who injects anaesthesia) will decide the type of anaesthesia suited for you. You will either get general anaesthesia, this will keep you asleep throughout the surgery, or spinal anaesthesia, this will be injected in your back to desensitize your lower body.
- Your surgeon will make a deep cut on the front of your knee.
- He/she will decide how much of your bone (wedge) is to be removed based on the affected region and mark the outline of the accurate measurements (size) of the wedge to be removed using guidewires.
- Then, the surgeon will remove the outlined part with an instrument called oscillating saw.
- Once the wedge is removed, he/she will fill the space using any one of the following methods:
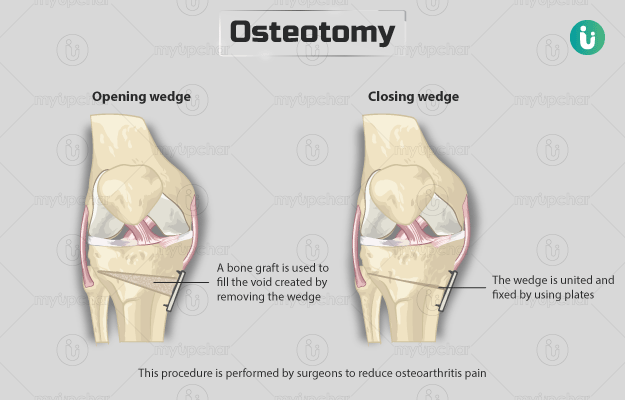
- Closing wedge: In this procedure, the bone located above and below the wedge is united and fixed by using screws and plates, thus helping keep the bones together until they are healed properly.
- Open wedge: In this procedure, the wedge is kept open. A bone graft (an artificial bone or bone from your body) is used to fill the void created by removing the wedge.
- Finally, the surgeon will stitch the surgical incision and tissues together, and apply a bandage over it.
The complete procedure may take an hour or two. The duration of your hospital stay may vary based on your condition and health. You may be eligible for a same-day discharge after the surgery if you can:
- Comfortably get up and lie down on the bed without any assistance
- Walk confidently/comfortably with crutches
- Bear/manage pain with medicines
In certain cases, you may need to stay in the hospital for about two days. During the stay, a nurse or the medical team will teach you the effective use of crutches. You will have a splint or brace around your joints for protection after the surgery.
How to care for yourself after osteotomy?
Your recovery period can last from three to six months after the surgery as per your condition.
Once you are home, you will need to care for yourself in the following ways:
- You will need crutches for at least for four to six weeks until you can comfortably bear your weight (or walk on your own) on your legs. Your doctor will advise you on when to stop using the crutches.
- Your doctor will prescribe painkiller medicines to help you in relaxing or managing the pain after the surgery. You can also use ice packs or cooling devices for this.
- You can walk, hike, or swim after the surgery; however, distance running or contact sports such as football should be avoided for a few weeks. Vigorous activities should be avoided until six to nine months after the surgery.
- You can resume driving six to 10 weeks.
- Rehabilitation - Your physiotherapist will suggest a few exercises to speed up your recovery.
This surgery can delay your need to undergo joint replacement surgery for up to 10 years.
When to see the doctor?
Visit or call your doctor directly if you experience any of the following symptoms after the surgery:
- Nausea or vomiting
- Fever
- Chills
- Cough
- Swelling, redness or pain at the surgical region
- Bleeding or leakage from the surgical cut
- Chalky white, black- or blue-coloured appearance of the leg, foot or toes
- Chest pain
- Breathing difficulties
- Desensitization or tingling in your legs, toes or feet
What are the possible complications/risks of osteotomy?
This surgery is known to carry the following risks:
- Stiffness in joints
- Blood clots in your leg
- Infection
- Bleeding
- Allergic reactions
- Breathing problems
- Failure to fix the bone during the surgery
- Nerve or blood vessel injury
When to follow up with your doctor after an osteotomy?
After your discharge, a follow-up appointment will be scheduled at two weeks for checking your wound and at six weeks to examine your joint (with an X-ray) and assess the success of the surgery. The surgeon will guide you in when you can fully bear weight on your joint and start further rehabilitation exercises.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
Doctors for Osteotomy

Dr. Manoj Kumar S
Orthopedics
8 Years of Experience

Dr. Ankur Saurav
Orthopedics
20 Years of Experience

Dr. Pritish Singh
Orthopedics
12 Years of Experience

Dr. Vikas Patel
Orthopedics
6 Years of Experience
References
- Royal Berkshire Hospital [Internet]. NHS Foundation Trust. National Health Service. UK; Osteotomy: high tibial (valgus) osteotomy and distal femoral (varus) osteotomy
- Cleveland Clinic [Internet]. Ohio. US; Knee osteotomy
- Frederick Azar S. Terry Canale James Beaty. Campbell’s operative orthopaedics. 13th ed. Philadelphia, PA: Elsevier; 2017
- National Health Service [Internet]. UK; Osteoarthritis
- Hospital for Special Surgery [Internet]. New York. US; Femoral Osteotomy
- Sarwar S, Lu J, Marcella C, Ji ML. Indications and clinical outcomes of high tibial osteotomy: a literature review. J Orthop Muscular Syst. 2019; 2(1):1007
- Beth Israel Lahey Health: Winchester Hospital [Internet]. Winchester. Maryland. US; Knee osteotomy
- Orthoinfo [internet]. American Academy of Orthopaedic Surgeons. Rosemont. IL. US; Osteotomy of the Knee.