Summary
One of the most common types of cancer in women is cancer of the ovaries. Ovaries are a pair of small female reproductive glands, which are connected to the womb by a pair of tubes (fallopian tubes). They store and supply eggs, which are important for a woman to conceive. Currently, the screening methods for Ovarian cancer are limited and diagnosis is usually delayed. Hence, prevention remains the most important focus of this disease. Women are most likely diagnosed at an advanced stage of cancer. Therefore, it makes the initial treatment difficult and its success rate, lower. In this scenario, surgery can be a part of both prevention (in women who are at high risk) and treatment of ovarian cancer. Screening is often carried out to assess the stage and type of ovarian cancer and can be used to plan successive surgeries to complete the treatment. It is carried out by a gynaecologist (a doctor who specialises in women’s health). You may either have a laparoscopy (surgery in which a camera is inserted through one of the cuts made and is used to visualise the insides of the body while performing the surgery) or laparotomy (done with a long, vertical cut from your bellybutton to your bikini line). The current standard treatment in India is maximal debulking surgery and tailored platinum-based chemotherapy. The surgery may be followed by a combination of other treatment methods, such as radiotherapy and chemotherapy. Taking care of the wound, diet, physical exercise, and medication play an important role in deciding the outcome of the surgery. Certain complications, such as bleeding, infection, clot formation, and so on may occur but can be managed effectively.
- What is ovarian cancer surgery
- Why is ovarian cancer surgery done
- Preparations before ovarian cancer surgery
- How is ovarian cancer surgery done
- Post-surgical care
- अंडाशय कैंसर की सर्जरी के बाद सावधानियां
- Risks and complications of ovarian cancer surgery
- Follow up after sugery
- Support after surgery
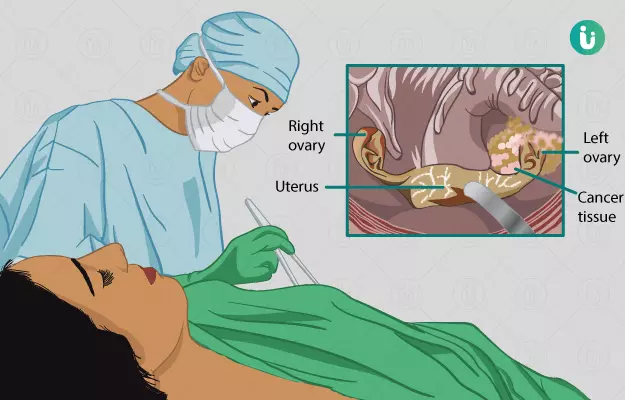
What is ovarian cancer surgery
The major role of ovarian cancer surgery is to remove the cancerous or affected part inside the female reproductive system. The surgical procedures that involve treating ovarian cancer include: cutting and joining of the tubes (fallopian tube ligation) and hysterectomy (removing the uterus but not the ovaries). This is done because sometimes, the origin of ovarian cancer lies in the womb. Overall, this surgery is done to make you cancer-free, improve your overall health and ensure it doesn't come back.
Why is ovarian cancer surgery done
The main aim of ovarian cancer surgery is to remove the growing cancer tissue in the ovaries. Other things that make it necessary to carry out this procedure are:
- Prevent the growing tumour from impinging on and damaging the surrounding tissue.
- To check the growth of cancer into the fallopian tubes and womb.
- Avoiding the side effects of excessive hormones produced by the tumour that not only affects the digestive system but also help cancer cells grow at a faster speed.
- To prevent the spread of ovarian cancer to other body parts through the bloodstream or lymphatic fluid (the fluid that carries waste from tissues to be filtered in the small swollen structures called lymph nodes).
Preparations before ovarian cancer surgery
Before your doctor finalises the surgery date, he/she may ask you a few questions, such as:
- Have you ever been hospitalised in the past for the same condition?
- Are you taking any medications for any other medical condition, such as diabetes, high blood pressure, thyroid diseases, liver disease, kidney disease, heart disease or any blood clotting problems?
- Are you allergic to any medications or numbing agent?
- Have you ever had surgery in the past? Was it successful? How was your recovery period? What problems did you face?
After conducting a physical examination of your whole body, your doctor may advise a few investigations and tests to assess your condition and see if you're fit for surgery. these tests include:
- Blood tests
- Urine tests
- Ultrasound of the lower belly
- X-ray
- ECG or Echo to test for heart function
- Breathing or lung tests
- MRI or CT scan
- Testing for allergy to any numbing agents, and so on.
Once the test reports are out, the surgeon will assess the findings and proceed further.
Cancer can be a life-changing and emotionally overwhelming diagnosis, however, it is strongly recommended that you seek as much information as possible to make a better, informed decision before treatment. The following questions must be asked to your doctor:
- What kind of ovarian cancer do I have?
- How much has cancer spread beyond the ovaries?
- What is the current stage of cancer and what does it mean in terms of treatment and overall outcome of the treatment?
- What all tests will be needed to understand the condition?
- What is the cost and insurance coverage of the available therapies?
- Will I be able to get pregnant after the therapy?
While deciding on treatment?
- What treatment options are there and which is the best one suited for me?
- What is the basis of recommending the procedure by you?
- Should I go for a second opinion? Or can you recommend a specialist for me?
- What will your treatment aim to achieve?
- How much time do I have to decide on the treatment?
- How can I prepare yourself for the treatment?
- What is the duration of the procedure? Where will it take place? Who all will be there to attend to me?
- The risks involved alongside the benefits are equally important to be addressed. Thus you can ask about the potential complications.
- What could be the best ways to reduce the harmful effects?
- For how long and by how much will your local activities be affected, such as work, exercise, family life, hobbies and so on?
- What are the chances that cancer will come back after the treatment?
- What will be the next step if cancer comes back?
How is ovarian cancer surgery done
It involves complete removal of the cancerous cells and surrounding tissues from the ovaries. The type of surgery needed depends on the spread of cancer in the body. It is usually treated and looked after by a team of gynaecologic oncologist (a cancer doctor), radiation oncologist, and medical oncologist. These doctors specialize in treating cancer. Other specialists may include physicians, nurses, psychologists, sex counsellors, and other health professionals.
There are different operations for various stages and types of ovarian cancer. Therefore, your doctor will carry out tests to detect the stage of cancer to plan the type of operation you will need.
Often, the operation may involve one of the following:
Removal of the womb:
- Total Abdominal Hysterectomy (TAH)
It involves removing both of your ovaries and the womb. - Bilateral Salpingo-oophorectomy or BSO
In this, the removal of both the ovaries and tubes is done on both sides. - Omentectomy
This refers to the removal of any infected part near the ovaries or cancer spread to adjacent organs (for example, removal of fatty layer over the end of intestine/bowel).
Fertility Conservation:
In this operation, ovaries and tubes will be removed only partially, and the womb will be left intact. This procedure is done if you are at the initial or starting stage of this cancer. After this procedure, you will most likely be able to get pregnant. However, if further samples detect that cancer has spread, this will mean that you need a second operation.
Debulking Surgery:
This is considered to be the most successful operation in treating ovarian cancer completely. Although, there may be some factors related to the complexity of cancer that may cause it to come back. This is the procedure of choice when cancer has spread to other areas in the hip and lower belly region. The aim of this surgery is to leave behind no visible cancer or tumours larger than 1 cm (known as optimally debulked). This procedure will include the removal of ovaries, tubes, womb, and part of your lower digestive system (for example, large or small intestine).
In severe cases, the large intestines and stool collection area cannot be tied back together after the tumour is removed. Therefore, an opening in the large intestine is made to hang the bag out from the skin; this is used to collect the bowel waste in it. Later on, it is reattached to its former position. Special care must be given to you in this either in the hospital or at home. People undergoing this surgery usually have a better outcome (prognosis) than those with partial surgeries.
Other organs that may need removal within this procedure include the colon (a part of the large intestine), a piece of the small intestine, a part of the gallbladder (a small organ present below the liver, which releases bile for fat digestion) along with the placement of a thin tube called catheter, and the spleen and/or the gallbladder, as well as part of the stomach, liver, and/or pancreas. However, this is done only in a few cases.
Surgery for epithelial cell tumour:
This procedure usually involves ‘staging’ and ‘debulking process’. Staging is a process where the surgeons and specialists categorise the tumour and examine them during surgery prior to their removal. This is important to plan future surgeries and to understand the spread of cancer so that you can be fully treated. If there is fluid accumulation in your lower belly or the space in the belly, it will be removed by your surgeon. The surgeon may "wash" the inside of your belly with salt water (saline) and collect this fluid. He or she may also take tissue samples from different areas inside the belly. All the tissue and fluid samples that are taken during the operation are sent to a lab for testing to look for cancer cells.
Surgery of ovarian germ cells and stromal cells:
The main goal at this stage is the removal of cancer completely. The ovarian germ and stroma cell (cells that produce eggs and keep them protected) cancer is usually present in one of the ovaries and hence, it may be advised to just remove the affected side. Sometimes, as a precaution, once you have your final pregnancy, surgery to remove the remaining ovary, the other fallopian tube, and the uterus may be recommended for both germ cell and stromal ovarian tumours.
Overall, the total cost of ovarian cancer surgery depends on the type and extent of spread of cancer and may range between 3,00,000-3,50,000 INR.
Post-surgical care
Once you've shifted to the recovery room, painkillers and antibiotics may be prescribed. Once you are discharged, your doctor may advise you to perform lighter exercises. You will need 3-7 days of hospital care after surgery. An important outcome of the removal of both ovaries is ‘early menopause’ or ‘end of periods’, which will cause respective bodily changes in you. Inability to have a baby can be emotionally straining and must be discussed with partner or family members.
Before you are discharged, speak with your doctor and ask the following questions:
After treatment
- What kind of diet is allowed or should be avoided?
- Limitations on activities?
- What all symptoms should be watched for?
- What type of exercises will be good for me?
- How to know if cancer has come and what should one do?
- What further options will be considered if cancer comes back?
Risks and complications of ovarian cancer surgery
There are certain risks and complications that decide the outcome of the surgery. Most of them are not very serious, however, a few are life-threatening. These complications include:
- Bleeding
- Infections
- Decreased gut activity leading to delayed bowel movement and waste removal.
- Blood clot formation in the leg veins
- Fever
- Formation of an abnormal opening in the digestive tract or urinary system
- Pneumonia
- Sutures might give way
- In severe cases, death may also occur if the complications are not managed in time.
Follow up after sugery
After your surgery, you will be advised to visit your surgeon to get your wound checked. You must ask questions about your condition and how it is proceeding. You will be informed about your condition and the status of cancer. You may often need more treatment after surgery as a precaution like chemotherapy, radiation therapy, hormonal therapy or sometimes a second surgery depending on the condition. Regular tests and check-ups will be advised and any new symptoms must be shared with your doctor.
Support after surgery
Self-help
In the end, after an overwhelming period of treatment and living with this condition, you are likely to have some mental and emotional reactions to surrounding around you. You may also develop depression once you're diagnosed with this condition. All these can affect important everyday functions like eating, sleeping or working, which cause tiredness and body’s poor immune response to fighting the disease. You are advised to go for counselling and therapy in order to keep yourself mentally and emotionally healthy.
Support groups
After the treatment, there are groups that help people who have been through the ‘same’, to come together and share their experiences, It is reassuring and comforting to share worries with people who understand your condition.
Surgery Cost In Your City
References
- NHS UK. Ovarian Cancer: Overview. Health A to Z. 2017 Jan 30. Accessed on 2019 May 23.
- Stewart C, Ralyea C, Lockwood S. Ovarian Cancer: An Integrated Review. Seminars in Oncology Nursing. Volume 35. Issue 2. 2019. Pages 151-156. ISSN 0749-2081
- Vinotha T, Anitha T, Ajit S, Rachel C, & Abraham P. The Role of Completion Surgery in Ovarian Cancer. Journal of obstetrics and gynaecology of India, 66(Suppl 1), 435–440. (2016). PMID: 27651643
- Swanson C.L. & Bakkum-Gamez J.N. Options in Prophylactic Surgery to Prevent Ovarian Cancer in High-Risk Women: How New Hypotheses of Fallopian Tube Origin Influence Recommendations. Current Treatment Options in Oncology. 2016 Mar 31.
- Walker, J. L., Powell, C. B., Chen, L. , Carter, J. , Bae Jump, V. L., Parker, L. P., Borowsky M. E., and Gibb R. K. Society of Gynecologic Oncology recommendations for the prevention of ovarian cancer. Cancer. 2015. 121: 2108-2120. PMID: 25820366
- Royal college of Obstetricians and Gynaecologists. Fertility Sparing Treatments in Gynaecological Cancers. Scientific impact paper. February 2013. Access date 2019 May 25
- Schorge, J. O., McCann, C., & Del Carmen, M. G. Surgical debulking of ovarian cancer: what difference does it make?. 2010. Reviews in obstetrics & gynecology, 3(3), 111–117. PMID: 21364862
- Maria E.L. van der Burg, Mat van Lent, Marc Buyse, Anna Kobierska, Nicoletta Colombo, Giuseppe Favalli, Angel J. Lacave, Mario Nardi, Josette Renard, Sergio Pecorelli. The Effect of Debulking Surgery after Induction Chemotherapy on the Prognosis in Advanced Epithelial Ovarian Cancer. The Gynaecological Cancer Cooperative Group of the European Organization for Re
- Yao T, Stephanie R. DeJong, Michaela E. McGree, Amy L. Weaver, William A. Cliby, Kumar A. Frailty in ovarian cancer identified the need for increased postoperative care requirements following cytoreductive surgery. Gynecologic Oncology, Volume 153, Issue 1 (2019) Pages 68-73 ISSN 0090-8258
- Purushothaman Natarajan, Sian E. Taylor, John M. Kirwan. Ovarian cancer: current management and future directions. Gynaecology & Reproductive Medicine, Volume 28, Issue 6, 2018, Pages 171-176, ISSN 1751-7214
- U.S. National Library of Medicine. Surgical Complications Related to Primary or Interval Debulking in Ovarian Neoplasm (SCORPION). NIH. 2011 Oct 28.
- Le, T., Kennedy, E. B., Dodge, J., & Elit, L. Follow-up of patients who are clinically disease-free after primary treatment for fallopian tube, primary peritoneal, or epithelial ovarian cancer: a Program in Evidence-Based Care guideline adaptation. 2016. Current oncology (Toronto, Ont.), 23(5), 343–350.
- Kathleen Ell, Nishimoto R, Mediansky L, Mantell J, Hamovitch M. Social relations, social support and survival among patients with cancer. Journal of Psychosomatic Research. Volume 36, Issue 6.1992. Pages 531-541,ISSN 0022-3999
- Price, M.A., Butow, P.N., Bell, M.L. et al. Helplessness/hopelessness, minimization and optimism predict survival in women with invasive ovarian cancer: a role for targeted support during initial treatment decision-making?. Support Care Cancer. Springer Link. 2016 Jan 6. 24: 2627.