Summary
Clitoris is a small, sensitive structure of the external genitalia in women. It is comparable to the male penis and is responsible for pleasure during sexual activity. It is located at the upper junction of the inner vaginal lips and is protected within the outer lips of the vagina. Clitoridectomy is the removal of the entire clitoris. This surgery is done for the treatment of reproductive cancers (mostly invasive cancers) and if there is enlargement or necrosis (death of the tissue) of the clitoris. The surgery involves clamping and removal of the clitoris. Some complications associated with clitoridectomy include pain, reduced sexual appetite and libido, bleeding from the incision and urinary tract infections.
Clitoridectomy is also performed as a part of female genital mutilation (FGM) in some regions of the world. The World Health Organization advocates against any kind of FGM procedures.
- What is clitoridectomy?
- Why is a clitoridectomy recommended/done?
- Who can and cannot get clitoridectomy?
- What preparations are needed before clitoridectomy?
- How is clitoridectomy done?
- How to care for yourself after clitoridectomy?
- What are the possible complications/risks of clitoridectomy?
- When to follow up with your doctor after a clitoridectomy?
What is clitoridectomy?
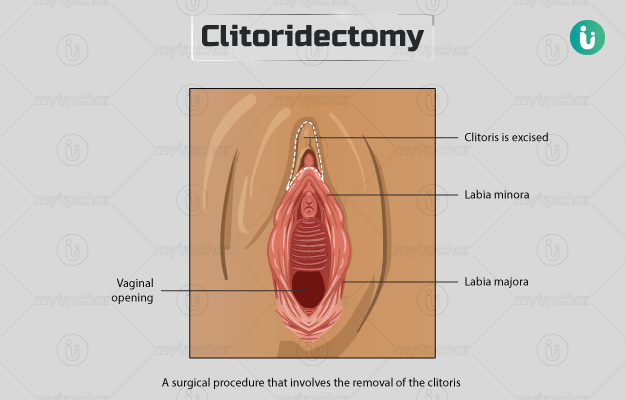
Clitoridectomy is a surgical procedure that involves the removal of the clitoris - which is a small, sensitive, erectile structure of the external genitalia in women located at the head of where the inner lips (labia minora) of the vagina meet.
Just like male penis clitoris in women is responsible for pleasure during sexual activity. The external, visible portion of the clitoris is called the glans (enlarged end). It is 1-1.5 cm (0.5 inches) in length and about 0.5 cm in diameter and is full of nerve endings. The glans is supported by a cylindrical structure called the shaft. The clitoral hood or the prepuce covers the entire structure. The clitoral shaft contains two spongy structures (corpora cavernosa) that fill with blood and cause the clitoris to become erect during sexual arousal. From each side of the clitoral shaft emerge root-like structures called the internal crura that connect to the pubic bones in the pelvis. The crura also fill up with blood when a woman is sexually aroused.
In some cultures, the clitoris is removed as a part of cultural or religious practices in which female genitalia are removed or cut. The cutting or partial or total removal of female genitalia for non-medical reasons is called female genital mutilation (FGM) and is considered a human rights violation. The World Health Organization (WHO) is opposed to all forms of FGM.
Why is a clitoridectomy recommended/done?
The medical reasons for the removal of clitoris are as follows:
- If the clitoris has necrosis, i.e., the tissue shows signs of death because of insufficient blood supply. These signs can be seen on the outer lips of the vagina as well.
- Damage to the clitoris or the nearby organs due to an injury. Also, certain radiation therapies to the pelvis affect the clitoral tissues, which may, therefore, need to be removed.
- Reproductive cancers that are likely to spread.
- Enlarged clitoris due to some drugs or production of excess sex hormone by the adrenal glands located on the kidneys.
Who can and cannot get clitoridectomy?
There are no contraindications for clitoridectomy that is done for medical issues.
Clitoridectomy for non-medical reasons should not be performed as per WHO.
What preparations are needed before clitoridectomy?
Pre-surgical evaluation for clitoridectomy will depend on the conditions such as the person’s age and existing medical conditions, e.g., obesity among others.
- Before a clitoridectomy, your doctor will advise you to undergo a general evaluation and a biopsy (evaluation of the diseased tissue) in cases of invasive cancer.
- As a part of pre-surgical tests, you will undergo tests such as a chest X-ray, electrocardiogram and blood tests.
- A healthy balanced diet and aerobic exercises are recommended for 30 days before the surgery.
- Cut down alcohol or smoking (if you do) when the surgery is planned.
- Do not eat or drink anything after midnight, the night before your surgery.
- Sleep early and well prior to your surgery.
- Take a bath before you go in for surgery but do not use any lotions, deodorants or powder after you shower.
- Do not wear any contact lenses while going in for surgery. Opt for glasses instead.
- Wear comfortable clothing. Do not wear jewellery, metal objects or prosthetic devices.
You must inform your doctor if you:
- Take any prescription or over-the-counter medications, blood-thinning medications, pain killers, anti-inflammatory medications or supplements (herbs, vitamins, minerals). You will be advised on how to continue with these medications before your surgery.
- Have any implant such as a pacemaker in your body.
- Have allergies to latex or any other materials that may be used during the surgery.
- Have allergies to any medicines used for anaesthesia
- Have shortness of breath while sleeping
- Take vitamin E, as it can increase the risk of bleeding
How is clitoridectomy done?
Before the surgery, you will be taken to the operating room and will be made to wear compression boots on your lower legs. These boots will inflate and deflate to allow blood circulation in your legs.
You may be given general anaesthesia to reduce pain. An IV line would be attached to your arm/hand to administer fluids during the surgery. A breathing tube will be placed in your windpipe through your mouth. A Foley catheter will be placed in your bladder to drain urine. Here is the procedure for a medical clitoridectomy:
- Your feet will be raised and your legs will be spread open for access. In cases of malignancy, the surgeon may first remove the lymph nodes in your groin region as well (called inguinal lymphadenectomy).
- The clitoris end will then be clamped and removed. To stop the bleeding, the surgeon would apply a pressure bandage. He/she will then close the incision with sutures. To ensure that all malignant or cancerous tissue is removed, the surgeon may excise the tissue slightly beyond the actual malignant regions.
After the surgery, while in the hospital:
- Your pulse, oxygen level and blood pressure will be monitored.
- You will not be allowed to sit until your incisions have healed. Thereafter, an inflatable ring will be given to you to sit on.
- You will be given pain medications to help control the pain.
- A catheter or drainage tube will still in be in place to drain urine from your bladder.
How to care for yourself after clitoridectomy?
Here are some things that your doctor would ask you to keep in mind when you
- The incisions and sutures to your clitoris might loosen with time. You may even see a reddish liquid oozing from them.
- You must keep your incisions clean with a small squirt bottle having a nozzle especially after you urinate or defecate.
- Use a hand shower to gently wash the area at least twice a day.
- You can shower with soap and water each day.
- Air dry the incision with gentle dabbing using a towel; do not rub.
- Wear loose clothing that lets the area be open.
- Eat a healthy balanced diet and drink plenty of liquids that do not contain caffeine or alcohol.
- You may be advised to elevate your feet, given diuretic medications (to induce urine), and compression stockings so that there is less fluid build-up in your body.
When to see the doctor?
You should see your doctor if you:
What are the possible complications/risks of clitoridectomy?
Clitoridectomy can have some immediate health risks and several long-term complications that can affect a women’s physical, and sexual health and wellness through life.
- Severe pain and swelling
- Reduced sexual sensitivity- reduced libido, sexual desire and pleasure, pain during sex, decreased lubrication, reduced orgasms
- Excessive bleeding – haemorrhage, if the clitoral artery or blood vessel is affected.
- Infection
- Problems with urination
When to follow up with your doctor after a clitoridectomy?
Your first follow up will be within two to four weeks of surgery. During this visit, your incisions will be evaluated and the staples, drains or sutures may be removed. Your doctor will let you know about the further follow-ups on this visit.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- Azadzoi KM, Siroky MB. Neurologic factors in female sexual function and dysfunction. Korean J Urol. 2010 Jul;51(7):443-9. PMID: 20664775
- Jones R, Lopez K. Human Reproductive Biology. 4th ed. Academic Press; 2014. Chapter 2, The female reproductive system; p.23-50.
- Graziottin A, Gambini D. Handbook of Clinical Neurology. Elsevier; 2015. Chapter 4, Anatomy and physiology of genital organs – women. Volume 130, p.39-60
- World Health Organization [Internet]. Geneva (SUI): World Health Organization; Health risks of female genital mutilation (FGM)
- Hoffman B, Schorge J, Schaffer J, Halvorson L, Bradshaw K, Cunningham F. Williams Gynecology. 2nd ed. New York: McGraw-Hill Medical; 2012.
- Izett S, Toubia N. 2000. Women and Health. Academic Press; 2000. Chapter 32, Female circumcision/female genital mutilation. p.404-419.