Summary
Rectopexy is a surgical procedure that is done to restore a person's rectum to its normal position. The procedure is done to treat conditions like rectal prolapse, rectocele and enterocele. The conditions are not life-threatening, but cause embarrassing symptoms and deteriorate the quality of life.
During the surgery, the rectum will be pulled to its normal position and fixed with stitches and sterile, netted sheets called mesh. In some cases, a part of the large intestine will also be removed to help improve bowel movements. The surgery takes about two hours, and you will be discharged in about one to three days after the procedure.
- What is rectopexy?
- Why is rectopexy recommended?
- Who can and cannot get rectopexy?
- What preparations are needed before rectopexy?
- How is rectopexy done?
- How to care for yourself after rectopexy?
- What are the possible complications/risks of rectopexy?
- When to follow up with your doctor after a rectopexy?
What is rectopexy?
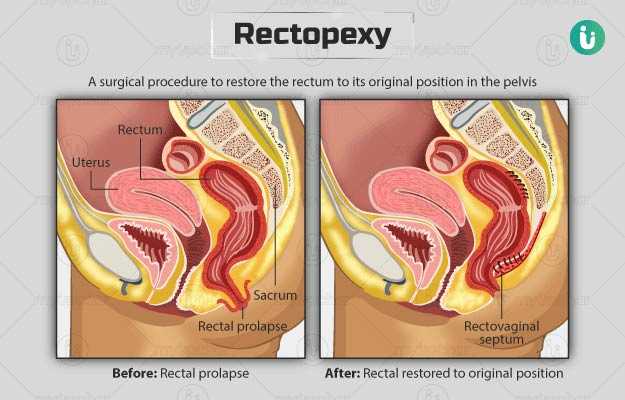
Rectopexy is a surgical procedure to restore the rectum to its original position in the pelvis.
Rectum is a part of the large intestine along with the cecum, colon, and anus. Cecum is the passage that receives almost digested food from the small intestine and then passes it into the colon. The latter absorbs nutrients and water from the digested food and passes the remaining waste (stool) to the 6 inches long tube at the end of the large intestine, i.e., the rectum. Rectum stores the stool until you are ready to pass it through the anus, the opening through which stools exits the body.
A group supporting muscles help keep the rectum in its original position within the pelvis. However, certain conditions such as tissue damage during childbirth, the subsequent need to strain during bowel movements due to constipation, or ageing can weaken these muscles. This causes the rectum to collapse into itself or protrude outside the anus. This condition is called rectal prolapse. Individuals with this condition usually lose control over their bowel movements. Although rectal prolapse is not life-threatening or dangerous, it can have a significant effect on your quality of life. The three types of rectal prolapse include:
- Partial/mucosal prolapse: The inner lining of the rectum protrudes out of the anus.
- Complete/external prolapse: The entire wall of the rectum comes out of the anus.
- Internal/incomplete prolapse: The rectum prolapses within the pelvis and does not protrude out of the anus.
The condition is treated initially with dietary modifications and other home treatments. However, if it does not improve with other treatments, a rectopexy is advised.
During the surgery, the rectum is pulled and fixed in its original position with stitches or mesh. A mesh is a sterile, netted sheet made of either biological tissue or synthetic material. Meshes made of biological tissue are safer than the synthetic ones. Sometimes, a part of the colon is also removed during the surgery.
Why is rectopexy recommended?
The surgery is most commonly recommended in individuals with rectal prolapse. Some symptoms of the condition include:
- Leakage of stool, blood, or mucous from the anus
- Bright red tissue protruding out of the anus
- Inability to empty the bowel completely
- Urgency to empty bowel
- Pain, irritation, and itching around the anus
Apart from rectal prolapse, rectopexy is done to treat the following conditions:
- Rectocele: In this condition, the rectum bulges into the vagina, Symptoms of rectocele are:
- Constipation
- Difficulty emptying the bowel completely
- Frequent urge to empty the bowel
- Pain in the rectum
- Pain during sexual intercourse
- Enterocele: In this condition, the intestine descends into the pelvis. Symptoms of this condition involve:
- Pain in the lower back
- Urine leakage
- Bulging in the vagina
- Frequent infections in the bladder
- Problems inserting tampons
Who can and cannot get rectopexy?
The contraindications to rectopexy include:
- Internal rectal prolapse with minimal bowel dysfunction
- Pregnancy
- Morbid obesity
- Severe intra-abdominal adhesions (scar tissue inside the abdomen)
- Active inflammation in the inner lining of the rectum
- High-grade endometriosis
- Absence of anatomical problems within the pelvis
- History of sigmoid peri-diverticulitis or pelvic radiotherapy
- Psychological instability
What preparations are needed before rectopexy?
Your surgeon will ask you to visit the hospital one to two weeks prior to the surgery for a preoperative assessment, wherein you will need to share the following details:
- Your medical history
- History of any allergies
- Whether you are pregnant
- A list of medicines that you take, including herbs and over-the-counter medications
Your doctor will conduct a physical examination and order the following tests:
- Blood tests
- Pregnancy test
- Electrocardiogram
- Proctogram (a test to study the working of the bowel and muscles within the pelvis)
- Formal anal manometry (a test to measure the pressure of the muscles that guards the anal opening)
- Colorectal transit study (a test to measure the ability of the colon to pass stool)
- Colonoscopy (a procedure that involves the use of a long, flexible instrument to look at the inner lining of the rectum)
Additionally, you will be given the following instructions:
- Discontinue the use of blood thinners like aspirin, warfarin, or ibuprofen. The surgeon will inform you about the medicines that you can take until the day of the surgery
- Fast from midnight before the surgery. Fasting is essential to prevent vomiting (risk of general anaesthesia) during the surgery.
- If you are a regular smoker, the surgeon will ask you to stop smoking.
- Do not drink alcohol on the day of the surgery or a day before.
- Drink about 1.5 litres of non-caffeinated fluids daily, and increase your fibre intake to soften your stools and ease bowel movements in the days leading to the surgery.
- Take a shower before you arrive at the hospital on the scheduled day of the surgery to minimise the risk of infections. Also, remove all nail polish, body piercings, and make-up.
- Arrange for a friend, family member, or responsible adult to drive you home after the surgery.
You will have to sign an approval form to grant your permission for the surgery.
How is rectopexy done?
After you arrive at the hospital, the hospital staff will ask you to undress and wear a hospital gown. You will be asked to wear special stockings to prevent blood clots. An intravenous (IV) line will be started in your arm or hand to supply essential fluids and medicines during the surgery. You will need to take an enema before the procedure to empty your bowel. The surgery involves the following:
- An anaesthetist will give you general anaesthesia (a sleep-inducing medicine).
- The surgeon will perform the surgery either by the traditional abdominal approach or the minimally invasive approach. The abdominal method involves a single large incision (cut) on the lower abdomen. In a minimally invasive approach, a small cut is made near the belly button to insert a laparoscope, followed by two to three small incisions in the abdomen to insert small surgical tools. A laparoscope is a thin, long camera that takes images of your internal organs and projects them onto monitors.
- The surgeon will then locate the rectum and free it from the nearby organs (vagina in women and prostate and bladder in men).
- He/she will gently lift your rectum back into its original position within the pelvis and fix it in place using stitches and/or mesh.
- Once the rectum is secured, the surgeon will clean your pelvis and close the abdominal cuts with dissolvable stitches.
Two commonly performed techniques for rectopexy are:
- Rectopexy with bowel resection: In this type of rectopexy, a section of the colon is removed to improve bowel function. This is usually done to treat long-term constipation.
- Ventral mesh rectopexy: Here, a mesh is stitched to the front wall of the rectum after separating it from nearby organs. The mesh is further fixed to the sacrum (the bone at the back of the pelvis) to secure the rectum in its normal position.
The minimally invasive approach is preferred over an open approach since it is associated with lesser pain, shorter hospital stay and recovery period. The surgery lasts for about two hours. You will be discharged in about one to three days after the surgery. During your hospital stay, you can expect the following:
- Immediately after the procedure, you will be taken to the recovery ward, wherein your vital signs will be regularly monitored.
- You will be supplied oxygen through a mask.
- A flexible tube will be inserted in your bladder to measure urine output, which will be removed on the day after the surgery.
- You will have an IV line in your arm or hand. The line will supply fluids and keep you hydrated until you are able to drink well on your own.
- The hospital staff will encourage you to get out of the bed and walk around soon after the surgery. This will promote recovery.
- Painkillers and laxatives will be given to you to provide relief from discomfort and ease bowel movement.
How to care for yourself after rectopexy?
The surgeon will provide some of the following instructions to take care of yourself at home after the surgery:
- You will need to take laxatives regularly for six weeks after the surgery to loosen your bowels. However, if you feel that the bowels are too loose, gradually decrease your laxative intake.
- Continue taking painkillers to ease the discomfort that you may experience. Avoid opiate drugs such as codeine as they can harden your stools.
- Do not perform strenuous exercises like running or lift heavy objects for at least six weeks following the procedure.
- Do not indulge in sexual activity for at least four weeks after the surgery.
- Drink a lot of non-caffeinated drinks and eat a high-fibre diet after the surgery.
- Avoid driving for at least two weeks after the surgery.
- Avoid swimming and excessive sitting or walking until the operated area has completely healed.
- You will need to rest for about four weeks at home before resuming work.
When to see the doctor?
Contact the surgeon at the earliest if you experience any of the following symptoms:
- Heavy bleeding
- Increased pain
- Fever
- Difficulty urinating
What are the possible complications/risks of rectopexy?
The potential complications/risks associated with rectopexy include:
- Infection at the operated site
- Bleeding
- Formation of a bulge at the operation site
- Constipation
- Chest infection
- Formation of blood clots
- Recurrence of the condition
Some rare risks associated with the surgery include problems with erection and ejaculation, erosion/infection of the mesh, long-term pain, and holes in the wall of the rectum.
When to follow up with your doctor after a rectopexy?
Your surgeon will ask you to visit the hospital six to eight weeks after the surgery where he/she will examine the operated area.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Find Proctologist in cities
Surgery Cost In Your City
Doctors for Rectopexy

Dr.P.S.Shah
Proctology
16 Years of Experience

Dr. Satyam Supare
Proctology
10 Years of Experience

Dr. Priyaranjan Tiwari
Proctology
10 Years of Experience

Dr. Sukrant Sharma
Proctology
7 Years of Experience
References
- Cleveland Clinic [Internet]. Ohio. US; Laparoscopic Rectopexy
- Canadian Cancer Society [Internet]. Toronto. Canada; The colon and rectum
- Royal Berkshire Hospital [Internet]. NHS Foundation Trust. National Health Service. UK; Rectal repair using keyhole surgery (laparoscopic rectopexy)
- Michigan Medicine [internet]. University of Michigan. US; Rectal Prolapse
- American Society of Colon and Rectal Surgeons [Internet]. Illinois. US; Rectal Prolapse Expanded Version
- Better health channel. Department of Health and Human Services [internet]. State government of Victoria. Australia; Rectal prolapse
- University Hospitals Plymouth NHS Trust [Internet]. National Health Service. UK; Laparoscopic Ventral Rectopexy
- Norfolk and Norwich Hospitals [Internet]. NHS Foundation Trust. National Health Service. UK; Abdominal rectopexy operation for rectal prolapse
- Royal Devon and Exeter Hospital [Internet]. NHS Foundation Trust. National Health Service. UK; Laparoscopic Ventral Mesh Rectopexy
- Mercer-Jones MA, et al. Consensus on ventral rectopexy: report of a panel of experts. Colorectal Dis. 2014 Feb;16(2):82–88. PMID: 24034860.
- Hernandez A, Sherwood ER. Anesthesiology principles, pain management, and conscious sedation. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 14.
- Miller RD, ed. Miller's Anesthesia. 9th ed. Philadelphia, PA: Elsevier Saunders; 2019
- Guy's and St. Thomas' Hospital: NHS Foundation Trust [Internet]. National Health Service. UK; Ventral Mesh Rectopexy