Summary
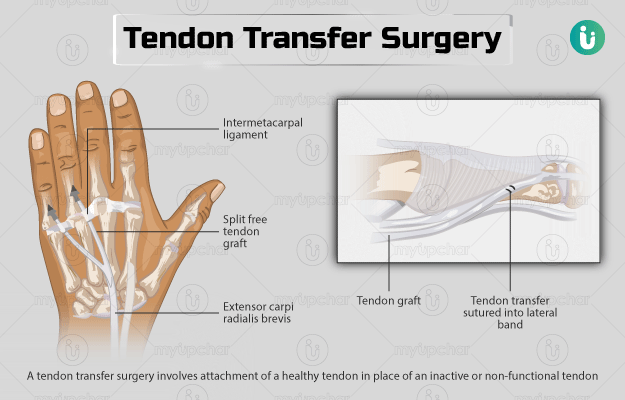
A tendon transfer surgery involves attachment of a healthy tendon in place of an inactive or non-functional tendon. The procedure is carried out to restore loss of movement of a joint.
Before the surgery, your doctor will ask you about your medical history, medications that you take, and your lifestyle habits. You will need to fast starting from midnight before the surgery until you are given permission to eat or drink after the procedure. The surgery may either be done under general, local or regional anaesthesia. After the surgery, you will need a plaster cast to protect the surgical area for a while. Recovery after the surgery may include a set of exercises recommended by a physiotherapist. You will need a follow-up to get your stiches removed and plaster cast changed a few weeks after the operation.
- What is tendon transfer surgery?
- Why is tendon transfer surgery recommended?
- Who can and cannot get tendon transfer surgery?
- What preparations are needed before tendon transfer surgery?
- How is tendon transfer surgery done?
- How to care for yourself after tendon transfer surgery?
- What are the possible complications/risks of tendon transfer surgery?
- When to follow up with your doctor after a tendon transfer surgery?
What is tendon transfer surgery?
A tendon transfer surgery is conducted to replace an inactive or non-functional tendon with a healthy one. A tendon is a tough cord that connects muscles to bones. Togather with muscles, tendons allow for smooth movement of joints. A tendon transfer surgery may be done if a tendon is diseased or if a ruptured or lacerated muscle cannot be repaired, leading to loss of muscles and tendon movement. The surgery may also be done if you have a nervous system disorder that causes you to lose muscle function. It helps to restore muscle movement and increase muscle function.
Why is tendon transfer surgery recommended?
Your doctor will recommend this surgery if you have a damaged tendon in places such as your wrist, thumb, or leg. A tendon or muscle can be damaged due to the following conditions:
- Nerve injuries that cause conditions like foot drop. In such conditions the injured nerve cannot send signals to the muscles, which causes paralysis of the affected muscles and loss of muscle function.
- Nervous system disorders like spinal muscular atrophy or cerebral palsy
- Rheumatoid arthritis
- Fracture
- Polio or leprosy, rarely
- Birth defects like hypoplastic thumbs (underdeveloped thumb)
You may experience the following if you have a damaged tendon in an area:
Who can and cannot get tendon transfer surgery?
The relative contraindications (surgery can be performed but with suitable precautionary measures) for tendon transfer surgery include:
- Poor muscle strength
- Stiff joints
- Reinnervated muscles (in which nerve supply has been restored)
- Any underlying neuromuscular disorder
What preparations are needed before tendon transfer surgery?
The following preparations are needed before the surgery:
- Medical examination: Your doctor will conduct a physical examination and carefully review your medical history. You will have to undergo routine scans like ultrasound or magnetic resonance imaging test before the surgery. The tests are generally done at least two to three weeks before the operation. They allow the doctor to check if you have any other medical problems prior to the surgery.
- Medications:
- Fasting: You will be asked to fast from midnight before the surgery until you are permitted to eat or drink after the surgery.
- Lifestyle: You will need to modify some of your lifestyle habits. The most important one being quitting smoking for some time before the surgery. This will expedite your recovery after the surgery. If you consume alcohol, inform your doctor about it.
- Driving: Your doctor may ask you to avoid driving for a few weeks after the surgery. Therefore, you will need to arrange for a friend or family member to drive you home after the operation.
- Arrange someone for home care: After certain tendon transfer surgeries, you will need someone to assist you for a few weeks at home.
- Consent: You will be asked to sign a consent form (granting your permission) before the surgery. Make sure to read the form carefully and ask the surgeon if you have any concerns regarding the procedure.
How is tendon transfer surgery done?
Before conducting this surgery, an anaesthetist (a medical professional who administers anaesthesia) will give you one of the following types of anaesthesia.::
- General anaesthesia: This will keep you asleep during the surgery
- Local anaesthesia: It numbs the site of the surgery
- Regional anaesthesia: It will numb a large area of the body (such as the leg or arm)
The surgeon will decide the type of anaesthesia you will need. This depends on factors such as the location of your injury.
The surgery will be performed in the following manner:
- The surgeon will make several cuts on your skin to expose your muscle and tendon area.
- He/she will identify and remove (from a muscle that can function properly without it) a tendon from the area that can replace the damaged tendon.
- The surgeon will then put this tendon in the place of the diseased tendon and attach and fix it to the bone using a drill hole and a bone anchor (a device that connects soft tissue to bone).
- If required, multiple tendon transfers will be carried out at the same time.
- Finally, the medical team will close the incisions using stitches.
The procedure may take from 90 to 120 minutes. Your hospital stay will depend on which region of your body was operated. For example, if you undergo a tendon transfer in your ankle, you may require a hospitalisation of about two nights.
How to care for yourself after tendon transfer surgery?
Once you are home, you will need to take the following care:
- Plaster cast (a stiff shell that encases and stabilises a limb):
- You will have to wear a cast or splint to protect the surgical area for about one to two months. This is usually applied along with a dressing or padded bandage.
- Pain management:
- Your doctor may prescribe a few painkillers to reduce your discomfort for the first few days after the surgery.
- Your doctor may suggest you to keep the surgical area elevated for the first few days after the procedure to reduce the swelling over the surgical area.
- Wound area:
- Make sure to keep the operated site clean and dry.
- Avoid applying lotion, cosmetic products, or powder on the wound.
- You can take a shower on the day after the surgery. Showers are preferable to bathing in a bathtub. However, avoid soaking the incision site.
- Driving and work: Your doctor will tell you when you can resume driving or going back to work.
- You may need physiotherapy that includes various exercises for faster recovery.
When to see the doctor?
Visit or call your doctor if you are experiencing the following symptoms:
- Fever or chills,
- Redness, swelling, numbness, or tingling near the plaster cast area,
- Cold feeling or blue discolouration of the skin around the surgical area.
- The cast becomes soft, loose, cracked, or uncomfortable.
- Any discharge, foul smell, or wetness around the cast.
What are the possible complications/risks of tendon transfer surgery?
The possible complications of a tendon transfer surgery are as follows:
- Tendon adhesions (scar tissue formation in the tendon that restricts movement)
- Infection
- Deep vein thrombosis
- Nerve injury
- Stiffness, swelling, and pain
- Stretching or rupturing of the stitched tendon
When to follow up with your doctor after a tendon transfer surgery?
The surgeon will schedule a follow-up appointment about two weeks after the surgery to remove your stitches and change your plaster cast.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- American Society for Surgery of the Hand [Internet]. Illinois. US; Radial nerve and tendon transfers
- Massachusetts General Hospital [Internet]. Boston. Massachusetts. US; Tendon Transfer Surgery
- Royal Berkshire Hospital [Internet]. NHS Foundation Trust. National Health Service. UK; Surgery to repair/reconstruct the tibialis posterior tendon
- Krishnamurthy S, Ibrahim M. Tendon transfers in foot drop. Indian J Plast Surg. 2019 Jan;52(1):100–108. PMID: 31456618.
- Northwell Health [Internet]. New York. US; Tendon Transfer Surgery
- American society of podiatric surgeons [Internet]. Bethesda. Maryland. US; Tendon transfer…to do, or not to do?
- Smith SF, Duell DJ, Martin BC, Gonzalez L, Aebersold M, eds. Clinical Nursing Skills: Basic to Advanced Skills. 9th ed. New York, NY: Pearson; 2016:chap 26.
- Neumayer L, Ghalyaie N. Principles of preoperative and operative surgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 10.
- Zambouri A. Preoperative evaluation and preparation for anesthesia and surgery. Hippokratia. 2007 Jan;11(1):13–21. PMID: 19582171.
- Beth Israel Lahey Health: Winchester Hospital [Internet]. Winchester. Maryland. US; Tendon Repair