Summary
Occipital nerve stimulation is a procedure performed for the treatment of various types of headache disorders that do not show improvement with other kinds of therapy. It involves the implantation of thin wires called leads in the back of the head and a battery in the abdomen, upper buttock, or below the collar or shoulder bone. The leads and battery are connected by an extension wire that runs under the skin. The device works by sending mild electrical impulses to the brain that block pain signals; however, it does not relieve the underlying condition. People who undergo this procedure experience at least 50% reduction in pain and increased comfort level during daily activities. Different types of batteries are used in the procedure. A lithium-based battery has a lifespan of around three to five years while a rechargeable battery lasts for about seven to nine years, after which it needs to be replaced. This surgery is considered reversible as it does not damage any nerves in the brain.
- What is occipital nerve stimulation?
- Why is occipital nerve stimulation recommended?
- Who can and cannot get occipital nerve stimulation?
- What preparations are needed before occipital nerve stimulation?
- How is occipital nerve stimulation done?
- How to care for yourself after occipital nerve stimulation?
- What are the possible complications/risks of occipital nerve stimulation?
- When to follow up with your doctor after occipital nerve stimulation?
What is occipital nerve stimulation?
Occipital nerve stimulation (ONS) includes the implantation of a device system in the body to modulate nerve activity in the head and treat various headache disorders that do not respond to other therapies.
The device consists of the following components:
- Leads and electrodes: Leads are thin, insulated wires while electrode refers to the tip (end) of the lead that makes contact with the brain tissue.
- Extensions: The cables, available in various lengths, which connect leads to the battery.
- Anchors: It secures the extension and leads to nearby tissue.
- Battery (internal pulse generator or IPG): Lithium-based or rechargeable battery is used as a power source.
The device sends mild electrical impulses in the back of the head. Although the exact mechanism of working of the device is still unclear, several theories have been proposed. Some of these theories suggest that the stimulation of nerves by the ONS device slows down or stops the transmission of pain signals to the brain. The device does not treat the source of the pain; instead, it stops pain signals from an area to reach the brain. Majority of the individuals who undergo ONS experience at least 50% pain reduction. The device does not have any permanent effect on nerves; therefore, ONS is a completely reversible procedure.
Why is occipital nerve stimulation recommended?
ONS surgery is recommended to reduce the symptoms, especially pain, in individuals with the following conditions:
- Occipital neuralgia: The condition causes continuous ache with random pain that starts from the base of the head and extends to one or both sides of the head.
- Cluster headache: The condition causes sudden pain with a piercing or burning sensation on one side of the head and one or more of the following symptoms:
- Sweaty face
- Runny nose or blocked nose
- Red eyes
- Drooping eyelid (of one eye)
- Chronic migraine: Symptoms of the condition include:
- Hemicrania continua: The condition causes daily, continuous headache on one side of the head along with symptoms such as:
- Restlessness
- Runny or blocked nose
- Sweating or redness on the headache side of the face
- Cervicogenic headache: The condition is associated with symptoms such as:
- Headache (usually one-sided)
- Neck pain
- Headache that worsens with neck movements
- Decreased range of mobility of the neck
- Headache associated with chemotherapy
Who can and cannot get occipital nerve stimulation?
This surgery is not recommended in the following cases:
- Infection in and around the site to be operated
- During pregnancy
- Bleeding disorders
- Opioid use
- Arnold-Chiari malformation (a condition in which some of the brain tissue extends into the spinal canal)
- Presence of an electrical implant (like a pacemaker) that may interfere with the working of the ONS device
What preparations are needed before occipital nerve stimulation?
You will have to visit the surgeon a few weeks prior to the surgery for a preoperative assessment wherein the surgeon will ask you to share the following details:
- Your medical history
- History of any allergies
- Whether you are pregnant
- List of medicines that you take, including herbs and over-the-counter medications
You will be asked to fill in some questionnaires, and undergo the following tests to ensure your eligibility for the surgery:
- Blood tests
- Urine tests
- Pregnancy test
In addition, you will be given the following instructions to prepare for the surgery:
- Discontinue blood-thinning medicines (warfarin, aspirin, ibuprofen, etc.) a few days before the surgery.
- Remove body piercings, nail polish, and make-up before arriving at the hospital for the surgery.
- Arrange for a friend, family member, or responsible adult to drive you home after discharge.
- Stop smoking a few weeks prior to the surgery.
- Fast from midnight prior to the surgery. This will help prevent vomiting (risk of anaesthesia) during the surgery.
- You will have to sign an approval form if you agree to the procedure.
A trial will be conducted before the surgery with leads implanted under the skin on your head and an external battery. The trial will last for about four to seven days, and if it successfully reduces your symptoms, the surgeon will go ahead with the permanent implantation of the ONS device.
How is occipital nerve stimulation done?
After you arrive at the hospital, the hospital staff will provide a hospital gown. They will also connect an intravenous drip in your arm to supply essential medicines and fluids during the operation.
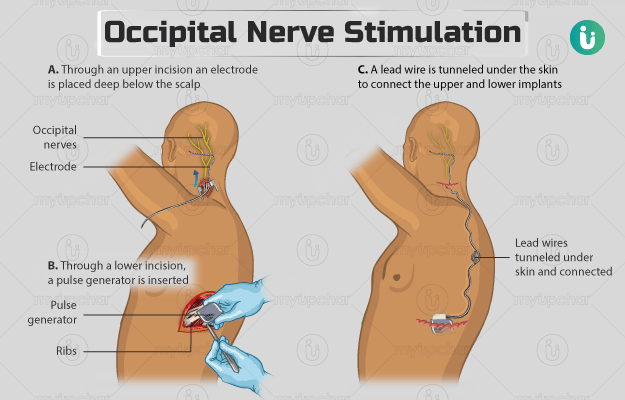
The surgery involves the following steps:
- Transfer to operation theatre: The hospital staff will take you to the operation theatre and place you on an operating table, either on your chest or side.
- Administration of anaesthesia: General anaesthesia will be administered to make you fall asleep. In addition, you will also be given local anaesthesia (numbing medicine) in the area where the leads and battery are to be implanted.
- Implantation of leads: Once the anaesthesia takes effect, the surgeon will make either of the following incisions:
- One on either side of your head, just below and behind your ear
- One small incision on the back of your head, about eight centimetres above the base of your neck. After making the cut, the surgeon will advance the electrodes towards the back of your head using X-ray guidance. Then, he/she will secure the leads with stitches.
- Implantation of the internal pulse generator (IPG): The surgeon will create a pocket at a site on your body to implant the battery and then attach the leads to the battery using extension wires passed through under your skin. He/she will then cover the implanted area with a dressing. Usually, the IPG is placed in one of the following sites: abdomen, upper buttock, or below the shoulder or collar bone.
The procedure lasts for about an hour. After the operation, the surgeon will take another skull X-ray to confirm the location of the implanted lead. When you wake up, you will feel tired, restless, and groggy and experience sore throat and dry mouth. These are side effects of the anaesthesia that fade within a few hours.
Apart from this, you will be given medicines to provide relief from any discomfort that you may experience post-surgery. You may need to continue your hospital stay for one to two nights. As it is not recommended to charge the device during the healing period, you will be discharged without programming the device; it will be set up during your follow-up visit.
How to care for yourself after occipital nerve stimulation?
Once you reach home, you will need to take the following care:
- Dressing: Keep the dressing on the site for implanted IPG for about three days. The hospital staff will give you extra dressings before discharging you from the hospital if you need to change them.
- Medicine: The surgeon will prescribe some painkillers for the initial few weeks or months after the surgery until the device is programmed.
- Shower: You will be allowed to shower from the next day of the surgery. However, avoid soaking the operated site until it completely heals.
- Physical activities: Avoid strenuous or vigorous activities until the surgical area heals completely. This usually takes about six weeks.
- Looking after the device: Do not rub the skin over the implanted site as it may damage the device. Avoid going through the security and theft detection device at the airport and shopping centres; instead, request for a hand search. However, if going through the security screening gate is mandatory, switch off the ONS device temporarily. Do not linger around the screening gates and devices.
- Driving: You will require about two weeks to turn your head freely without any restriction. The surgeon will allow you to resume driving thereafter.
- Work: Your doctor will suggest you to rest for at least four weeks before you go back to work. This period may change depending on the nature of your occupation.
It is normal to experience a comfortable tingling sensation when the device blocks the pain signals. The lifespan of a lithium-based battery is around three to five years while a rechargeable battery lasts for about seven to nine years. You will need to replace the battery thereafter.
Individuals who undergo this surgery report an improved comfort during daily activities post-surgery as the device provides at least 50% reduction in pain. However, you will have to continue your pain medicines even after the ONS to help with the pain relief.
When to see the doctor?
Contact the surgeon if you experience any of the following symptoms:
What are the possible complications/risks of occipital nerve stimulation?
The potential complications/risks associated with the surgery include:
- Infection in the operated site
- Headache
- Bleeding
- Allergic reaction to medicine or implanted material
- Increased pain or failure to relieve pain
- Malfunction of the device
When to follow up with your doctor after occipital nerve stimulation?
You will need to visit the hospital two weeks after the surgery to get the stitches removed and get the ONS device programmed. During the follow-up appointment, you will be given a controller to allow you to adjust the setting of the device.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
Doctors for Occipital Nerve Stimulation

Dr. Hemant Kumar
Neurology
11 Years of Experience

Dr. Vinayak Jatale
Neurology
3 Years of Experience

Dr. Sameer Arora
Neurology
10 Years of Experience

Dr. Khursheed Kazmi
Neurology
10 Years of Experience
References
- Sakharpe AK, Cascella M. Occipital Nerve Stimulation. [Updated 2020 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Stanford Healthcare [Internet]. University of Stanford. California. US; The Deep Brain Stimulator
- Oxford University Hospitals [internet]: NHS Foundation Trust. National Health Service. U.K.; Occipital Nerve Stimulation
- Lambru G, Matharu MS. Occipital nerve stimulation in primary headache syndromes. Ther Adv Neurol Disord. 2012 Jan;5(1):57–67.PMID: 22276076.
- American Association of Neurological Surgeons [Internet]. Illinois. US; Occipital Neuralgia
- National Health Service [Internet]. UK; Cluster headaches
- Cleveland Clinic [Internet]. Ohio. US; Chronic Migraine
- American Migraine Foundation [Internet]. New Jersey. US; Hemicrania Continua
- Hernandez A, Sherwood ER. Anesthesiology principles, pain management, and conscious sedation. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 14.