Summary
Orchiectomy is the surgical removal of either one or both testicles - male sex glands that are located behind the penis. It is commonly performed for treating testicular cancer but can also be done as a secondary procedure for prostate cancer treatment. to reduce the hormone (testosterone) levels and to avoid its recurrence. Testosterone promotes prostate cancer growth. Orchiectomy is also recommended as a part of gender change surgery.
In some cases, orchiectomy may be followed by another surgery to treat cancer that has spread to other parts of the body - abdominal lymph nodes for example. Therapies like chemotherapy and radiation therapy may also be recommended depending on the type of cancer.
After orchiectomy, reconstructive surgery with an artificial testicle may be advised to maintain the natural look of the genital. However, the decision is personal. The surgery may take about one hour and is performed under general anaesthesia. You may visit the doctor six weeks after the surgery.
- What is orchiectomy?
- Why is orchiectomy recommended?
- Who can and cannot get orchiectomy?
- What are the preparations needed before orchiectomy?
- How is orchiectomy done?
- How to care for yourself after orchiectomy?
- What are the possible complications/risks of orchiectomy?
- When to follow up with your doctor after an orchiectomy?
What is orchiectomy?
Orchiectomy is a surgery done to remove one or both male sex glands - testicles (testes).
Testicles are located in a pouch of skin (scrotum) below the penis. They produce sperms and the male hormone testosterone. Testosterone is essential for the development of the penis and testes in boys. It also determines bone growth, muscle development and other changes at puberty like the deepening of voice and appearance of pubic and facial hair.
Testosterone helps maintain fertility as it is responsible for sperm production and sex drive. Additionally, it maintains bone density and muscle strength in men.
Orchiectomy is most commonly done as a treatment for testicular cancer. It is also done for conditions like undescended testes.
The testes are formed in the abdomen when the baby is in the mother’s womb. They descend (move down) into the scrotum in 8th month of pregnancy. However, in babies that are delivered before 8th month of pregnancy (preterm babies), this fails to happen, and the testes remain in the abdomen or descend midway. They are called undescended testes and are associated with an increased risk of cancer.
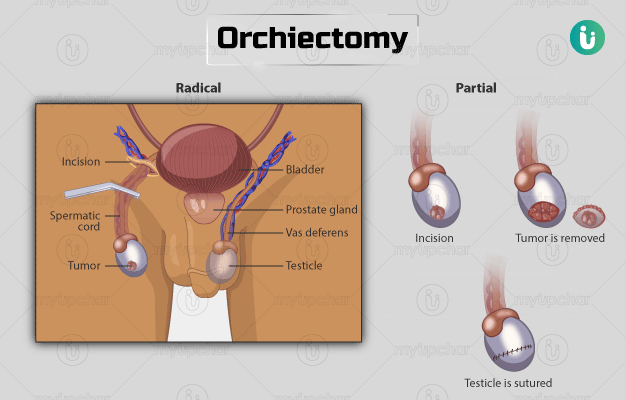
Orchiectomy can be done using different methods. The testes can be removed through a cut in the groin region (radical inguinal orchiectomy) or the scrotum (simple orchiectomy). The tissue lining the testes may be removed while preserving the testes (subcapsular orchiectomy). Sometimes, bilateral orchiectomy is also done, in which both the testes are removed.
Why is orchiectomy recommended?
Orchiectomy is most commonly done to remove the cancerous growths of testes. Doctors may recommend this surgery if a person at high risk for testicular cancer shows the following symptoms of (or has been diagnosed with) testicular cancer:
- Enlarged, swollen testicles with testes hanging lower than usual. Read more: Testicular swelling causes
- A sensation of heaviness or pain in the testes or scrotum.
- A lump on the testicle that may be painful or painless.
- Early puberty: Puberty changes in boys, e.g., growth of hair on the face and body, hoarsening of voice can occur at an early age due to certain types of testicular tumours (Leydig cell tumour) as they produce the male sex hormone, androgen.
- Breast enlargement or soreness: This may occur in certain types of cancer as the cancerous cells secrete female sex hormones (human chorionic gonadotropin and oestrogen).
If testicular cancer has spread to different body parts, symptoms may develop depending upon the organ involved. These involve lower back pain, chest pain, cough, vomiting blood, headache or abdominal pain in case of spread to the lymph nodes, lungs, abdomen, brain, and liver, respectively.
In some cases, diagnosis may be made accidentally when imaging tests are done for other conditions, as some men with testicular cancer may not present with any symptoms.
Risk factors for testicular cancer comprise:
- Age: It may affect males of any age; however, 50% of cases are seen in the age group of 20 to 34 years.
- History of testicular cancer: About 3% to 4% of people with cancer of one testis develop cancer in another testis later in life.
- Genetic disorder: A family history of specific genetic abnormalities (Klinefelter syndrome) can also cause increased precedence to testicular cancer.
- Undescended testes: About 3% of boys are born with undescended testes, and it increases the chances of developing testicular cancer.
- HIV infection: People with AIDS have increased chances of developing testicular cancer.
- Being of a certain race or ethnicity: Around 4 to 5 times increased occurrence is seen in American and European males as compared to Asian and African.
Orchiectomy is also recommended in men with the following conditions:
- Prostate cancer
- Cancer in undescended testes
- Severe trauma to the testicles
- Breast cancer
- Male-to-female transgender surgery, i.e., transgender orchiectomy surgery
Who can and cannot get orchiectomy?
It is essential to confirm the diagnosis of cancer before performing this surgery.
Orchiectomy is undesirable in certain types of cancers like epidermoid (lining of the scrotum) carcinoma.
Also, this procedure should not be performed at all in conditions like:
- Scrotal hematoma (accumulation of blood outside the blood vessel in the scrotum)
- Infection of the scrotum
- Inflammation of the testes (granulomatous orchitis)
- Adrenal rests (testicular tumour produced from adrenal embryonic rest cells)
- Leydig cell hyperplasia (increased number of interstitial cells of the seminiferous tubules that secrete testosterone)
- Certain types of cancer like myeloma and cancer that has spread from its original site to other parts of the body.
What are the preparations needed before orchiectomy?
Before the surgery, the following tests are done to confirm the diagnosis of testicular cancer/tumour:
- A thorough physical examination of the testicular lump followed by ultrasound is essential to support the diagnosis.
- Blood tests to identify tumour markers (blood tests to identify the presence of cancerous growth), i.e., beta-human chorionic gonadotropin, lactate dehydrogenase, and alpha-fetoprotein are also done.
- A small part of the lump or mass is removed for histopathology (microscopic examination by an ultrasound-guided percutaneous biopsy to help confirm the diagnosis and determine the type of treatment. It is minimally invasive and can be performed under local anaesthesia as an outpatient procedure.
There is a chance of spread of cancerous cells when a biopsy is done in cases of suspected testicular cancer. Therefore, orchiectomy is not only used as a part of treatment but also to confirm the diagnosis.
Once the diagnosis is reached, the following things need to be done before the surgery:
- You will be asked to sign a consent form, which gives the doctor approval to perform the procedure. Your doctor will explain the risks and effects of surgery and anaesthesia.
- He/she will also explain to you the option of using a prosthesis (artificial testes) to maintain the natural appearance of your genitals after orchiectomy. You can tell your doctor if you want to opt for it.
- You may ask all your questions at this stage – how will the surgery affect you in having an erection, your sperm count, any hormonal changes or fertility issues, as most of the people with testicular tumours needing orchiectomy are of young age groups.
- In the case of bilateral orchiectomy, it is essential to consult your doctor about sperm banking (storing frozen sperm cells) before the surgery if you wish to have children in the future.
- Avoid drinking or eating anything for a minimum of six hours before the procedure. Read more: Effects of alcohol on body
How is orchiectomy done?
Orchiectomy requires a short hospital stay (it is an outpatient procedure). After admission in the hospital, the surgery will be carried out in the operating room, and you will be given general anaesthesia (so that you fall asleep during the procedure) or regional anaesthesia for the surgery.
A healthcare practitioner will shave your scrotal region before surgery. A drip will be inserted in your arm, and monitoring devices will be attached to your body to keep tabs on your vitals (heart rate for example). The surgery will take 45 minutes to 1 hour.
Depending upon the diagnosis, one of the following procedures may be used:
- Radical inguinal orchiectomy: Most testicular cancers require a radical inguinal orchiectomy. In this surgery, the surgeon will make an incision in your groin region, remove the tumour along with the testes and the cord attached to it (spermatic cord) Spermatic cords are tube-like structures that are connected to the testes to maintain their position. These cords are removed to prevent the spread of cancer through blood and lymphatic drainage in the cord. The wound will then be closed carefully to prevent the development of hernia in the future.
- Simple orchiectomy: In a simple orchiectomy, testes will be removed by making an incision on the scrotum.
- Subcapsular orchiectomy: In this surgery, only the inner lining of testes will be removed (testosterone is made here), leaving the testes in place.
- Testis-sparing orchiectomy: This surgery is commonly done to remove the tumour mass if it is a benign (non-malignant) tumours with normal markers. In this surgery, the doctor will cut the tumour with clear margins and send it to the laboratory to look for possible signs of malignancy. At any slightest chance of malignancy on laboratory examination or risk of malignancy in the residual tumour, this surgery is followed by radical unilateral or bilateral (both testes) orchiectomy
- Bilateral orchiectomy: In this surgery, both the testes are removed by an incision made in the front of the scrotum. Bilateral orchiectomy is commonly done in prostate cancer to prevent future complications and to relieve its symptoms by lowering testosterone levels.
Depending upon the extent of the tumour, additional surgery may be done to remove the lymph nodes infected by cancerous metastasis, if any. Orchiectomy may also be followed by other therapies like chemotherapy or radiation therapy when needed.
Reconstructive surgery is mostly recommended by doctors wherein a testicular prosthesis (artificial saline implants) is placed in the scrotum to maintain the normal look of the genitals. However, it is your personal decision.
Orchiectomy is the most effective surgery in treating cancer of testes, especially if diagnosed at an early stage.
After the surgery:
Once the surgery is done, you will be transferred to the recovery room and monitored until the effect of the anaesthesia wears off. Then you will be shifted to a ward. You will have scrotal support (a special pair of underpants) in place to prevent bleeding and give support to the scrotum. You may also have a drip for the adequate supply of fluids until you start drinking. You will be asked to go home once you have started eating and have passed urine.
How to care for yourself after orchiectomy?
You will be given directions to take care of the wound as follows:
- Keep the wound area clean and dry
- Wash the wound daily by not directly applying soap to the incision
- Dressing needs to be done to collect any discharge from the wound area. The wound will heal and stop oozing after three to five days.
You will be given medications to prevent infection, constipation, blood clot, pain, and nausea. In the case of bilateral orchiectomy, you may also be given hormonal supplements to maintain testosterone levels.
You may take into consideration the following things at home:
- Wear a jockstrap or scrotal support to prevent swelling for at least three to five days after surgery. This also makes you comfortable and promotes healing.
- Use ice packs as indicated.
- Avoid strenuous work, lifting weights, or straining for stools for at least four weeks.
- Use a doughnut cushion when sitting for comfort.
- Try doing relaxation and breathing exercises
- You may need help to carry out your daily activity until complete recovery
Consult your doctor before resuming driving, work, and sexual activity. You can expect a full recovery by four weeks.
The benefits of orchiectomy are:
- Helps in relieving symptoms
- Long-term survival in people with prostate cancer
When to see the doctor?
Call the healthcare provider if you develop any of the following problems after surgery:
- Discharge or bleeding from wound even five days after surgery
- Swelling or redness at the site of the incision
- Fever
- Swelling of the scrotum
- Difficulty in urinating
What are the possible complications/risks of orchiectomy?
As with any surgery, orchiectomy also has risks and side effects associated with it. These include:
- Haematoma (bleeding in the scrotal sac). A large purplish scrotum may indicate it. It is normal for the scrotum to be tender and swollen for two to four weeks.
- Nerve injury at the time of removal of the spermatic cord. It is especially seen in individuals with the previous history of surgeries in the same region.
- Inguinal hernia (a soft tissue bulges out through a weak point in the abdominal muscles)
- Side effects of anaesthesia like fall in blood pressure, wheezing in chest, rash, or swelling.
- Localised infection
- Bleeding or clot formation
- Removal of testes causes male sex hormone deficiency leading to depression, hot flashes, mood swings, erectile dysfunction, infertility, enlarged breast, and loss of sex drive.
- Osteoporosis (bones become brittle and weak)
- Fatigue
- Weight gain
When to follow up with your doctor after an orchiectomy?
A follow-up visit is generally scheduled around 6 weeks after the surgery to check that the wound is healing well. You may need to visit the doctor regularly to check for recurrence of cancer.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
Doctors for Orchiectomy
Dr. Purushottam Sah
Andrology
40 Years of Experience

Dr. Anurag Kumar
Andrology
19 Years of Experience
References
- Oncolink [Internet]. Philadelphia: Trustees of the University of Pennsylvania; c2018. Surgical Procedures: Orchiectomy
- Harvard Health Publishing. Harvard Medical School [internet]: Harvard University; Testosterone — What It Does And Doesn't Do
- Johns Hopkins Medicine [Internet]. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System; Radical Orchiectomy
- American Cancer Society [internet]. Atlanta (GA). USA; Signs and Symptoms of Testicular Cancer
- UW Health: American Family Children's Hospital [Internet]. Madison (WI): University of Wisconsin Hospitals and Clinics Authority; Orchiectomy for Prostate Cancer
- Michigan Medicine: University of Michigan [internet]. US; Orchiectomy for Testicular Cancer
- Indiana University School of Medicine: Department of Medicine [Internet]. Indiana University. Indiana. US; Orchiectomy