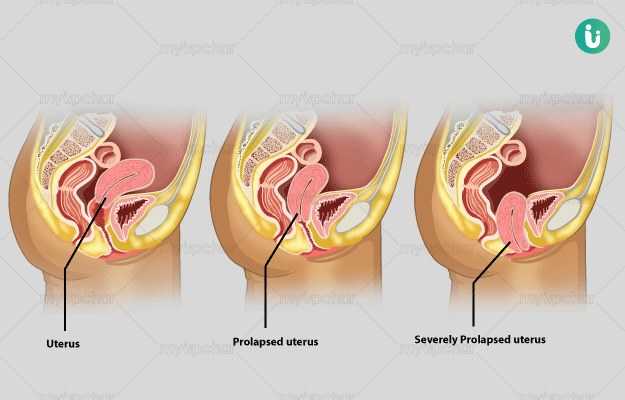
The female pelvic region contains the uterus (womb), the urinary bladder and the rectum. There are numerous muscles and ligaments present at the floor of the pelvis that provide some support and hold these organs in position.
A prolapse occurs when the pelvic floor muscles are weak and ineffective. As a result, one or more of the above-mentioned organs present inside the pelvis prolapses or drops down into a space called the vagina.
A prolapse can be classified based on how far the organ has dropped into the vagina. In certain situations, the prolapse can be to such an extent that the walls of the vagina or the uterus protrude outside the opening of the vagina.
Read on to know about uterine prolapse, including uterine prolapse during pregnancy and uterus prolapse due to old age.
Surgery for uterine prolapse
The goal of the surgery is to provide a definitive cure for uterine prolapse. Various operations can be performed, depending on the type and degree of prolapse. Laparoscopic or keyhole surgeries may be done in some cases. You should ask your doctor for the best possible option in your case. The various surgical procedures that can be performed may include the following:
- Vaginal repair operation: In this operation, your vaginal walls are reinforced, strengthened and tightened. This is achieved by making a tuck in your vaginal wall and applying sutures to hold it in place. The operation can be done via the vagina and does not require any incisions in the abdominal area. Sometimes, a mesh or a unique tape may be stitched onto the vaginal walls. There may be some complications, including mesh erosion through the vaginal wall. This would require further surgery and may involve sexual difficulties and pain.
- Hysterectomy or removal of the uterus: This is a very commonly performed surgery in patients with uterine prolapse. Indeed, uterine prolapse is the most common reason why women over 50 undergo a hysterectomy. It may also be performed in combination with a vaginal repair operation.
- Procedure to lift your uterus or vagina up: Numerous surgeries can be performed to lift the uterus and vagina up. These may include the following:
- Sacrohysteropexy: A unique mesh is usually used that performs the function of a sling to support and hold the uterus in place. One side of the mesh is attached to the cervix (neck of the womb) and the other is attached to the sacrum; that is, the bone at the back of the pelvis. This surgery requires an incision in the abdomen.
- Sacrocolpopexy: During this procedure, the vagina is lifted up and held in place by fixing it to the sacrum or the bone at the back of the sacrum. It requires a mesh to hold the vagina in place. This may be performed in combination with a hysterectomy. This surgery requires an incision in the abdomen.
- Sacrospinous fixation: During this procedure, the vagina is lifted up and attached to the sacrospinous ligament (a ligament in the pelvis). This procedure is performed through the vagina and does not require an incision in the abdomen. This procedure may also be done after a hysterectomy.
- Colpocleisis: This procedure involves the sealing of the vagina. This is a rare operation as it makes sex impossible. It is usually performed in old frail females. The patients should be informed about these consequences before the operation.
Patients are advised to stay in the hospital for a few days after surgery. Complete recovery is typically achieved in two to three months. Patients should not have sexual intercourse and should avoid lifting heavy weights during this period of time as the prolapse may recur.

 Doctors for Uterine prolapse
Doctors for Uterine prolapse  OTC Medicines for Uterine prolapse
OTC Medicines for Uterine prolapse