Summary
Bursectomy is the surgical removal of a bursa or bursae. Bursas are small fluid-filled sac within joints that reduces friction and enables the free movement of bones, muscles, and tendons.
This surgery is often recommended to treat Bursitis or inflammation of bursae. Bursae are inflamed either by wear and tear, infections, injuries, or underlying conditions such as gout, arthritis and diabetes. Bursitis can lead to swelling, discomfort, loss of movement, redness, and fever.
Conservative treatments of rest and anti-inflammatory medications help cope with bursitis. However, if the severity of inflammation and pain increase, a surgery may be indicated.
Bursae are located throughout the body – in the knees, shoulders, hips, and ankles. The location decides the type of bursectomy to be adopted. Bursectomy in the shoulder can be done with endoscopy and by the use of surgical tools that make the surgery minimally invasive. On the other hand, bursectomy in the knees involves making an incision to remove the bursae. Depending on the location of the bursa, a bursectomy can last from 30 minutes to two hours.
The complications involved in such surgeries may include extensive bleeding, infections, or formation of blood clots. A follow-up visit to the doctor is generally scheduled two to three weeks after the surgery.
- What is bursectomy?
- Why is bursectomy recommended?
- Who can and cannot get a bursectomy?
- What preparations are needed before bursectomy? - Bursectomy kaise hoti hai
- How is bursectomy done?
- How to care for yourself after bursectomy?
- What are the possible complications/risks of surgery?
- When to follow up with your doctor after a bursectomy?
What is bursectomy?
Bursectomy is the surgical removal of an inflamed bursa (a small sac within a joint, which is filled with fluid) or bursitis. Bursitis mostly affects the bursae in the elbows, shoulders, hips, knees, and feet.
The bursa is a small cushion-like structure, made of connective tissue and lined with synovial fluid (a viscous liquid that lubricates joints). They are located at places of possible friction, including between the bones and the adjoining soft tissues, bones and the muscles around the joints, and bones and tendons (the fibrous connective tissue that attaches muscles to bones). Bursae are vital to the human body as they reduce tension and wear and tear at points where the most friction occurs in a joint and provide free mobility to the skeletal body.
The bursa sac is made up of a semi-permeable membrane facilitating certain materials to move in and out of the membrane. There are 160 bursae present in the human body of varied shapes and dimensions.
In cases of an injury in the bursa, blood can accumulate within the sac and can cause irritation. Irritation of the bursae can cause inflammation. This condition is called bursitis.
Bursitis can occur by repetitive movements around the bursal area or a sudden injury. Inflammatory disorders, trauma, or infectious diseases are also the causes of bursitis. Additionally, the excessive use or damage to the bursa or surrounding joints, bones, muscles, and ligaments increases the risk of bursitis. Trauma to the bursa or, rarely, infection at the inflamed bursal site can lead to sepsis and cause septic bursitis.
Bursitis can be of two types – acute and chronic. Acute bursitis arises due to infection, direct trauma, or joint diseases by an accumulation of crystals at the joints (like in gout). It results in pain and limited mobility. Chronic bursitis occurs due to the immune response of the body, creating prolonged inflammation at certain sites, especially the joints (inflammatory arthropathies), overuse of affected joints. Often chronic bursitis may be painless, but thickening and swelling of the bursa can occur due to build-up of fluid.
The person is advised to rest as a treatment for bursitis. Additionally, antibiotics, non-steroidal anti-inflammatory drugs, stretching, and physiotherapy may be recommended. In some cases, surgery may be considered.
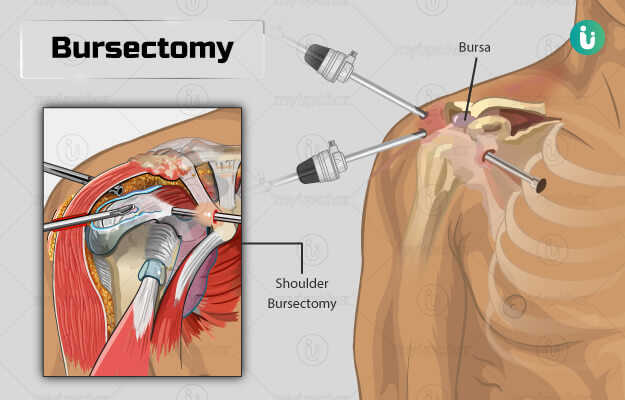
Bursectomy can be of two types:
- Open bursectomy: It allows direct visualisation of the bursae.
- Endoscopic (arthroscopic) bursectomy: In this method, multiple incisions are made in the skin, through which a camera (endoscope) and surgical tools are inserted to carry out the surgery.
Why is bursectomy recommended?
Bursectomy may be advised for the following symptoms in a bursa that indicate bursitis:
- Tenderness
- Discomfort
- Redness or swelling in the affected area
- Difficulty or loss of movement
- Fever
Who can and cannot get a bursectomy?
A bursectomy may be advised in individuals with the following conditions that can cause bursitis:
- Rheumatoid arthritis
- Scleroderma
- Osteoarthritis
- Gout
- Systemic lupus erythematosus
- Thyroid disease
- Diabetes
Bursitis can be treated depending on the duration of the condition, location of an inflamed bursa, and seriousness of the inflammation. Generally, it is treated with rest, ice, elevation, and compression (RICE), anti-inflammatory medications, painkillers, local applications in the form of patches, by drawing out the fluid collected in an inflamed bursa with a needle (needle aspiration), and corticosteroid injections. A bursectomy is generally recommended when these conservative treatments are unsuccessful.
Bursectomy is not advised as a standard treatment in people with gastric cancer.
What preparations are needed before bursectomy? - Bursectomy kaise hoti hai
Before you undergo a bursectomy, the following pre-surgical steps will be carried out:
- You may need to undergo some evaluations, namely ultrasound and X-rays of the bursa.
- Pre-operative safety evaluations like ECG, blood tests, and blood pressure checks will be performed.
- Inform your doctor if you take any medications, supplements or herbs. You may be asked to discontinue some of them a week before the surgery.
- Do not take antihaemorrhagic agents (medicines that prevent bleeding) a few weeks before the surgery.
- Inform the doctor if you smoke or drink and follow their advice on the steps to be taken prior to the surgery.
- On the night before your surgery, no food or beverages should be consumed.
You should arrange for someone to ride you home after the surgery.
How is bursectomy done?
Bursectomy can be carried out either under general anaesthesia (you will be asleep during the procedure) or local anaesthesia (only the part operated on is numbed, and the person remains awake) depending on the location of the inflamed bursa. It can be performed as an endoscopic or open bursectomy.
Endoscopic bursectomy: An inflamed bursa in the shoulder joint can be operated on by a shoulder joint endoscopy. Here is how this surgery is done:
- You will be made to lie down on your back (in a supine position) with a tourniquet placed near the surgical site. The tourniquet exerts pressure on the limb and surrounding region, thereby, reducing but not cutting off blood supply to the area.
- The skin above the affected joint will be sterilised, and the procedure will be performed under local anaesthesia. If pain is experienced, regional anaesthesia (that numbs a larger part of the body) may be used.
- Two portals of entry will be made, one towards the centre (medial) of the site and another towards the edge of the site (lateral).
- A small camera or endoscope (also known as an arthroscope) will be inserted through one portal to help in guiding the surgical instruments. A tool called a shaver that enables trimming and removing the fluid in the bursa will also be directed into one of the portals.
- After the surgery is complete, the openings will be sutured. Some drains will be retained for continued drainage; they will be removed the next day.
- This surgery is considered less invasive than open bursectomy, has a faster recovery and causes less discomfort. You will be allowed to go home the same day of the surgery.
Open bursectomy: This method is generally used when the inflamed bursa is on the knee or the elbow joint. Here is how an open bursectomy done:
- You will be made to lie down on your back (in a supine position) with a tourniquet placed near the surgical site.
- Under the effect of regional anaesthesia, an opening will be made on the skin over the affected joint.
- The bursa will be completely removed, and the region will be closed with absorbable stitches.
- A splash-proof dressing may also be applied to the wound, but it should still be kept dry for 10 days.
- The procedure may take from 30 minutes to two hours, which largely depends on where the bursa is located.
Post-surgery care:
- After the surgery, your blood pressure, breathing, and heart rate will be checked.
- An ice pack will be placed on the affected site to reduce swelling at the joint.
- Compression bandage will also be applied as a precaution against swelling and should be kept for at least three days.
- You will have to take a course of prophylactic antibiotics and medications for two days to prevent or reduce inflammation and cope with the discomfort.
- For a shoulder bursectomy, your arm will be placed in a sling, and you will need to keep the elbow perpendicular to the rest of your body to prevent pressure.
- You will be shown some physiotherapy exercises to help you recover and improve your joint health before getting discharged from the hospital.
- Additionally, the staff will demonstrate the use of any devices or braces that will assist you in your recovery and mobility.
How to care for yourself after bursectomy?
Post-surgical care at home is described as follows:
- The dressing should be kept clean and moisture-free. Take care that the wound does not get wet while bathing until the sutures are removed. Avoid any strenuous activity for a few days and activity that requires physical exertion until four to six weeks after surgery.
- Any pain related to the condition will get better in a few weeks, but swelling may take longer to go away fully.
- After the surgery, the wound dressing should be changed each day. The sutures will be removed at your next follow-up visit, two weeks after the surgery. You will then be allowed to resume a normal daily routine.
- You can begin work and indulge in sports-related activities after about 3-1/2 months of the surgery.
A bursectomy can help alleviate inflammation and pain in an individual with bursitis in whom conservative treatments have failed.
When to see the doctor?
Please visit a doctor if you experience any of the following symptoms:
- Continuous nausea or vomiting.
- Swelling, increased pain, redness, or excessive bleeding from the site of incision.
- A discharge from the incision site which may be foul-smelling.
- Breathlessness
- Symptoms of infection, including fever (> 101.5ᵒF) or chills.
- Pain that does not subside even with the pain medication.
- Lack of sensation or feeling of weakness in the joints or muscles around the affected bursa.
What are the possible complications/risks of surgery?
The complications of a bursectomy are as follows:
- Damage to nerves or blood vessels
- Formation of blood clots
- Profuse bleeding
- Infection
- Breakage of tools that are used to perform surgery, which is seldom
- Continued pain
- Slow healing
- Sinus formation (formation of a tunnel through the wound into soft tissue resulting in a dead space where abscess can form)
- Recurrence of bursitis
When to follow up with your doctor after a bursectomy?
A follow-up visit with your doctor for suture removal and a check-up will be scheduled two weeks after your surgery.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- Cooper University Healthcare [Internet]. New jersey. US; Bursectomy
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Bursitis: Overview. 2018 Jul 26
- Hirji Z, Hunjun JS, Choudur HN. Imaging of the bursae. J Clin Imaging Sci. 2011;1:22. PMID: 21966619.
- Mercadante JR, Marappa-Ganeshan R. Anatomy, Skin Bursa. [Updated 2020 Feb 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Williams CH, Sternard BT. Bursitis. [Updated 2019 Sep 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Doulens KM, Kuhn JE. Arthroscopic and open management of scapulothoracic disorders. In: Cole BJ, Sekiya JK. Surgical techniques of the shoulder, elbow, and knee in sports medicine, 2nd ed. Philadelphia: Elsevier Saunders; 2008: p. 326.
- Benenden Hospital [Internet]. The Benenden Healthcare Society Limited. York. UK; Bursectomy
- Beth Israel Lahey Health: Winchester Hospital [Internet]. Winchester. Maryland. US; Bursectomy.
- Mammoth Orthopedic Institute [Internet]. Mammoth Hospital. California. US; Post-operative Instructions: Excision of Prepatellar Bursa
- Meric G, Sargin S, Atik A, Budeyri A, Ulusal AE. Endoscopic versus Open Bursectomy for Prepatellar and Olecranon Bursitis. Cureus. 2018;10(3):e2374. Published 2018 Mar 27. PMID: 29805943.
- Nicholson Gregory P., Duckworth Monica A. Scapulothoracic bursectomy for snapping scapula syndrome. Journal of Shoulder and Elbow Surgery. 2002. 11(1): 80-85.