Summary
Leucorrhoea is a common and normal condition seen in women. It is the secretion of a transparent fluid or the mucus, which keeps the vagina moist and lubricated, and prevents vaginal infections.
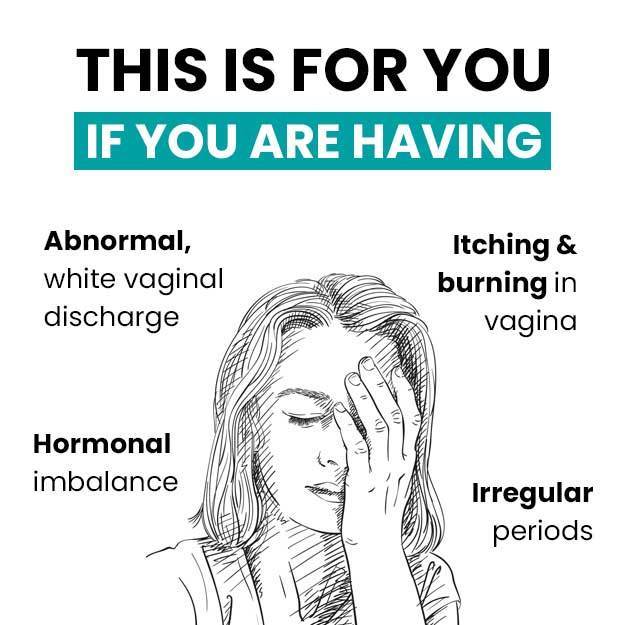
Leucorrhoea occurs due to fluctuations in hormonal levels during a woman's adult life from puberty to menopause. Symptoms of leucorrhoea, such as a non-itchy white discharge and a feeling of wetness, are harmless and can be resolved without any complications.
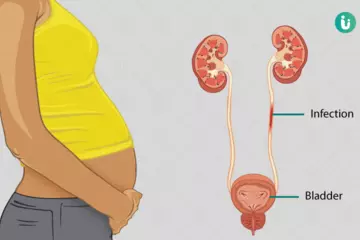
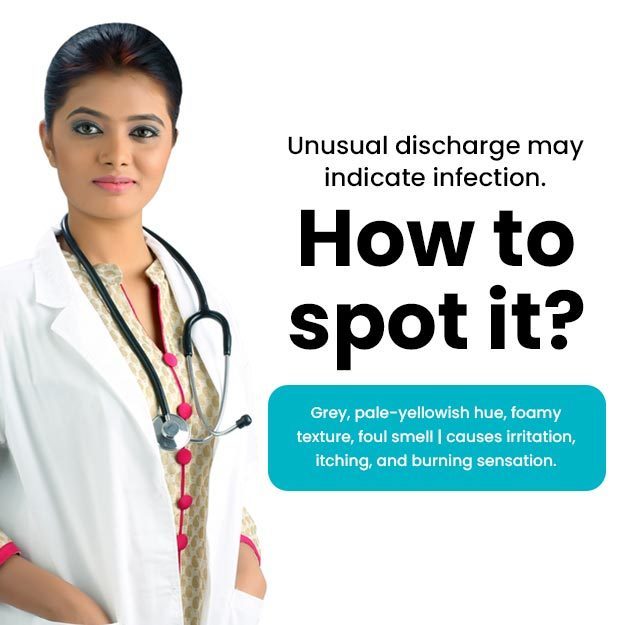
Causes of leucorrhoea include non-sexual as well as sexually transmitted infections.
In these cases, symptoms like itching, redness, bad odour, and discomfort or pain might be also be experienced.
Such infections need medications as well as other precautionary measures to prevent the transfer of infections or the development of complications. Leucorrhea doesn’t need treatment unless it is excessive or abnormal.

 Doctors for White Discharge (Leucorrhea)
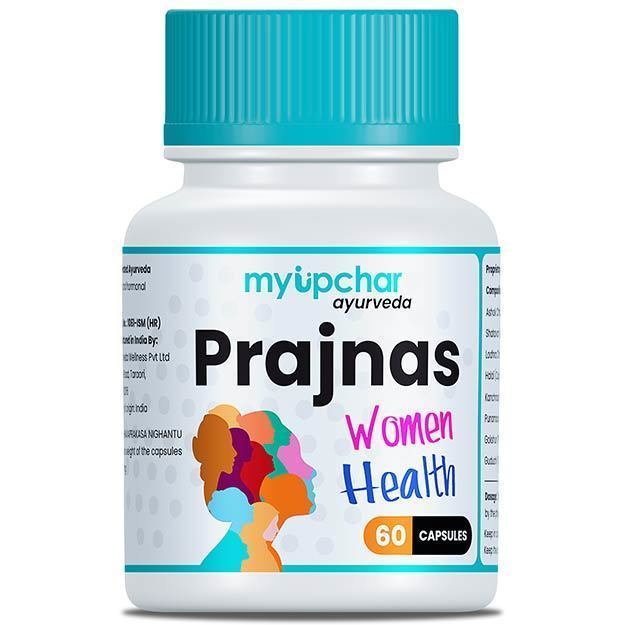
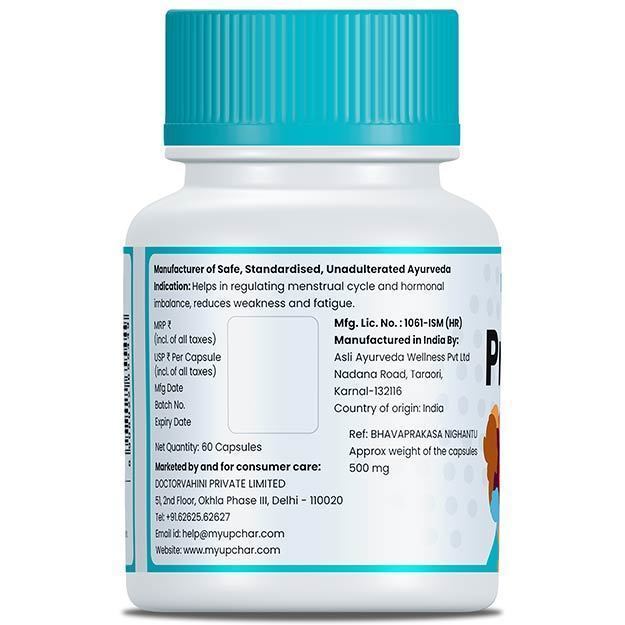
Doctors for White Discharge (Leucorrhea)  OTC Medicines for White Discharge (Leucorrhea)
OTC Medicines for White Discharge (Leucorrhea)
 White Discharge (Leucorrhea) articles
White Discharge (Leucorrhea) articles
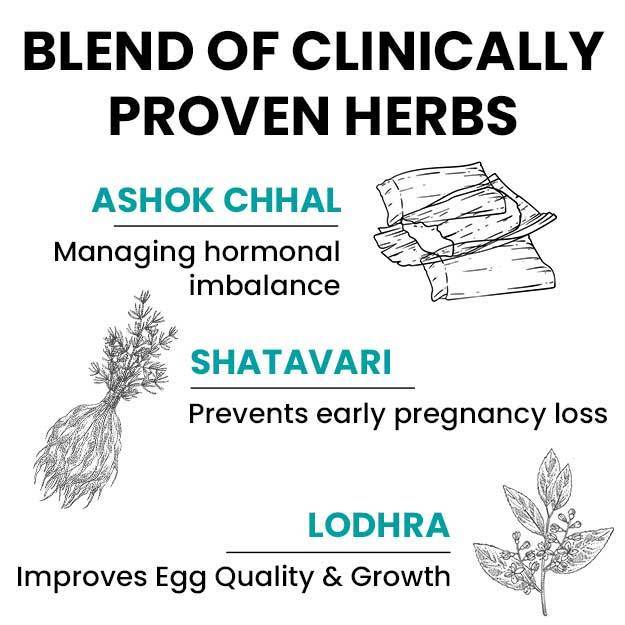
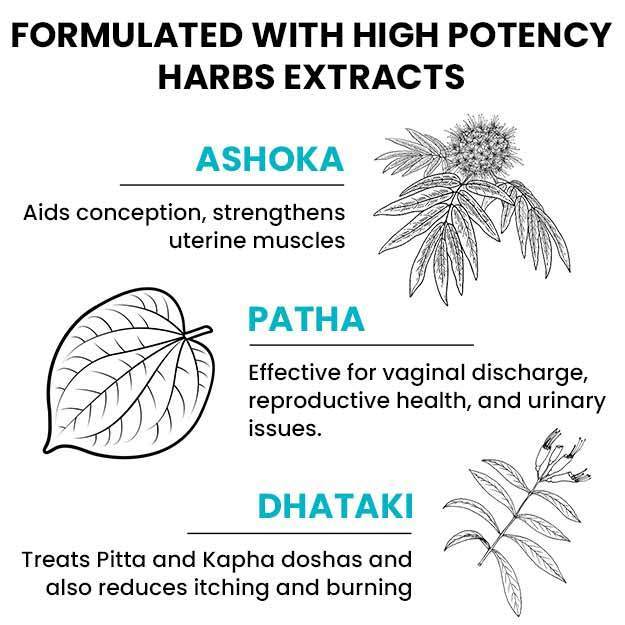
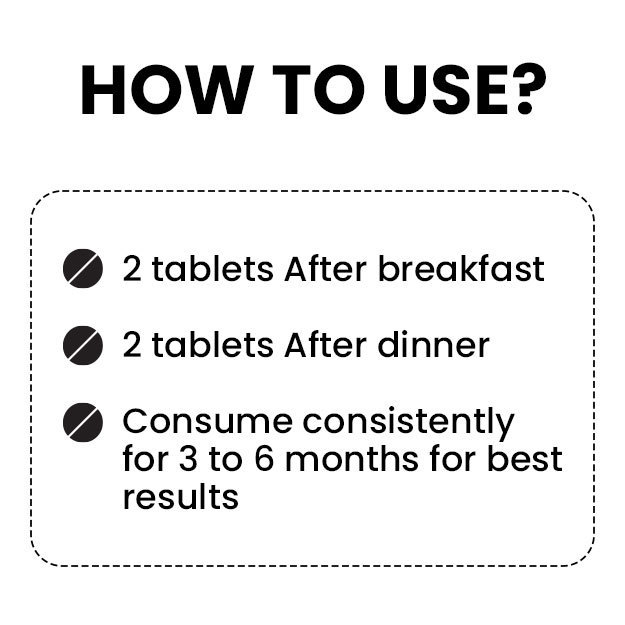
 Ayurvedic Treatment of White Discharge (Leucorrhea)
Ayurvedic Treatment of White Discharge (Leucorrhea)
 Diet for White Discharge (Leucorrhea)
Diet for White Discharge (Leucorrhea)
 Home Remedies for White Discharge (Leucorrhea)
Home Remedies for White Discharge (Leucorrhea)
 Homeopathic Treatment of White Discharge (Leucorrhea)
Homeopathic Treatment of White Discharge (Leucorrhea)

























 Dr. Vishal Makvana
Dr. Vishal Makvana

 Dr. Laxmidutta Shukla
Dr. Laxmidutta Shukla




 Dt. Akanksha Mishra
Dt. Akanksha Mishra