Summary
Arthroplasty is a surgical procedure wherein a diseased or damaged joint is resurfaced or removed and replaced by a plastic, metal, or ceramic substitute called prosthesis. The surgery is performed when the affected joint cannot be repaired by non-surgical options such as physical therapy and medicines.
Arthroplasty can be carried out in various joints including those in the shoulder, hip, elbow, and knee. The procedure usually lasts for one to three hours, and you will be discharged in around one to three days after the surgery. A physical therapist will visit you during the hospital stay and teach you exercises to perform at home. These will help promote recovery. After the surgery, you will experience relief from the joint pain and observe improved mobility in the affected joint.
- What is arthroplasty?
- Why is arthroplasty recommended?
- Who can and cannot get an arthroplasty?
- What preparations are needed before arthroplasty?
- How is arthroplasty done?
- How to care for yourself after arthroplasty?
- What are the possible complications/risks of arthroplasty?
- When to follow up with your doctor after an arthroplasty?
What is arthroplasty?
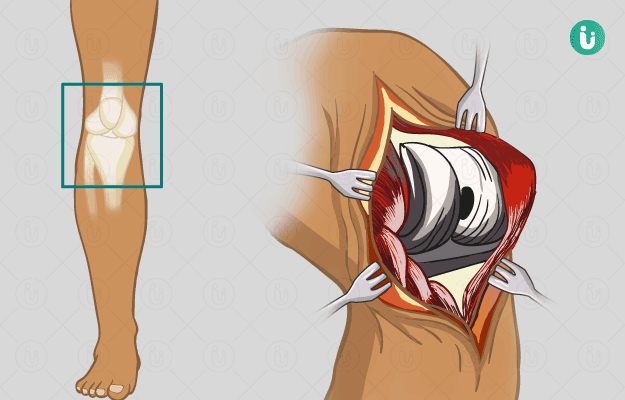
Arthroplasty is an orthopaedic surgery in which a damaged joint is resurfaced or replaced with a prosthesis (artificial substitute). The different types of arthroplasty include:
- Total arthroplasty: The entire damaged joint is removed and replaced
- Partial arthroplasty: The damaged part of the joint is removed and replaced
- Resurfacing arthroplasty: The damaged surface of the joint is resurfaced
A joint is an area where the ends of two or more bones meet. There are different joints in the body, of which some are fixed while others provide mobility to bones. The types of mobile joints in the body include hinge joint (knees, fingers, and elbows), ellipsoidal joint (wrists), ball-and-socket joint (hips and shoulders), and pivot joints (neck).
Certain joint conditions like fractures, arthritis and gout cause intense pain and affect the mobility of the affected joints. In arthroplasty, the affected/damaged joint is resurfaced or replaced to allow it to function like a healthy joint. The prosthesis used to replace the damaged part of the joint is usually made of plastic, metal or ceramics. Although knee and hip joints most commonly undergo arthroplasty, the surgery is also performed on other joints such as the wrist, ankle, elbow, or shoulder.
Why is arthroplasty recommended?
Arthroplasty is performed to provide relief from joint pain and disability that does not resolve with non-surgical treatments (medicines, physical therapy, weight loss, etc.). Conditions that require this surgery include:
- Osteoarthritis
- Septic arthritis
- Haemophilia
- Rheumatoid arthritis
- Bone dysplasia
- Lack of blood supply to the bone in the joint
- Loss of cartilage
- Gout
- Fracture
Troubled by obesity? Failed to lose weight? Now control weight easily by myUpchar Ayurveda Medarodha Weight Control Tablet. Get started today and take steps towards a healthy life.
Who can and cannot get an arthroplasty?
Arthroplasty is contraindicated in individuals with the following conditions:
- Sepsis (latent or active)
- Infection in the joint or elsewhere in the body
- Severe vascular dysfunction (dysfunction of arteries)
- Dysfunction of the extensor mechanism of the knee (muscles that extend the knee) – specific contraindication for knee arthroplasty
- Irreparable rotator cuff tear, brachial plexus palsy, or inadequate glenoid bone stock –contraindications for shoulder arthroplasty
What preparations are needed before arthroplasty?
You will have to visit the surgeon a few days prior to the surgery for a preoperative assessment wherein you will be asked to share the following details:
- Medical conditions (in case you have or had any)
- If have any allergies
- Pregnancy status
- List of medicines that you take, including herbs, vitamins, and non-prescription medications
A physical examination will be conducted, and you will have to undergo the following tests to help the surgeon look at your joint and ensure that you are physically fit for the surgery:
- Blood tests
- Urine tests
- Pregnancy test
- Cardiogram
- X-ray
In addition, you will be given the following instructions to help you prepare for the surgery:
- Discontinue aspirin, ibuprofen, warfarin, and other blood-thinning medicines several days to weeks before the surgery. You will be given a list of medicines to take on the day of the surgery.
- Stop smoking as it may delay healing.
- Inform the surgeon if you have a fever, cold, or flu on the days leading to the surgery. In this case, your surgery may be postponed.
- Fast from midnight before the surgery. Fasting is recommended before the surgery to prevent vomiting (risk of general anaesthesia) during the surgery.
- Shower and remove all make-up, body piercings, and nail polish before you arrive at the hospital on the scheduled day of the surgery.
- Arrange for a family member, friend, or responsible adult to drive you home from the hospital and help you in daily house chores for one to two weeks following the surgery.
- Meet a physical therapist prior to the procedure to plan for the rehabilitation programme following the surgery.
If you agree to the procedure, you will be asked to sign an approval form to give your consent.
How is arthroplasty done?
After you arrive at the hospital, you can expect the following:
- The hospital staff will ask you to undress and wear a hospital gown.
- An intravenous (IV) drip will be connected to a vein in your arm to supply fluids and medicines during the surgery.
- You will be asked to remove dentures, glasses/contact lens, or hearing aids.
The procedure usually involves the following steps:
- An anesthesiologist will administer general or regional anaesthesia to you. The former will put you in a deep sleep while the latter numbs the area of the body to be operated.
- You will be connected to devices that will measure your vital signs during the procedure.
- The hair over the area to be operated will be shaved off and then cleaned with an antiseptic solution.
- The surgeon will make a cut (incision) over the joint to be operated.
- In total and partial arthroplasty, the damaged/diseased joint will be removed and replaced with a prosthesis. In resurfacing arthroplasty, the damaged surface is trimmed and covered with a smooth metal shell.
- The surgeon will stitch the incision to close it and cover the area with a dressing.
The surgery will last for around one to three hours. After the procedure, the hospital staff will shift you to the recovery ward and later to a hospital room once your condition is stable. During your hospital stay, you can expect the following:
- You may feel tired, restless, and groggy. You may even experience a sore throat and dry mouth upon waking up after surgery. These are side effects of anaesthesia that will fade within a few hours.
- Your vital signs will be continuously monitored.
- You will be given medicines to provide relief from pain after surgery and antibiotics to prevent infection.
- Compression stockings will be put on your legs to prevent blood clots.
- An X-ray will be taken of the operated joint so the surgeon can examine the joint.
- You will be taught to use a spirometer, a device that will keep your lungs clear and prevent pneumonia.
- A physical therapist will meet you and teach you to sleep, sit, and stand comfortably. Additionally, you will be taught to use a cane, walker, or crutch if needed. You will be taught exercises to perform at home on your own.
You will be discharged in one to three days following the surgery.
How to care for yourself after arthroplasty?
You will be provided with the following instructions to care for the operation site at home:
- Keep the area of surgery clean and dry. Follow the instructions given by the hospital staff to change your dressing.
- Use a walker, crutch, or cane as instructed by the physical therapist or surgeon.
- Take the prescribed medicines as directed by the surgeon.
- Resume driving only after consulting the surgeon.
- Follow the exercise regimen recommended by the physical therapist.
- You may need to make some alterations at home to ease your recovery. Some of the modifications that you may need at home include:
- Safety handrails in the shower and along the stairs
- Stable chairs with arms, firm back, and seat cushion
- Dressing stick (a long, wooden stick with a special hook at its ends that helps in dressing-related tasks)
- Raised toilet seat
- Avoid lifting objects or indulging in activities that require you to bend or squat.
When to see the doctor?
Contact the surgeon if you experience any of the following symptoms:
- Fever with body temperature more than 101oF
- Chills
- Increased swelling, pain, warmth, or redness in the operated site
- Tingling or loss of sensation in the extremity of the affected joint
- Drainage from the incision
What are the possible complications/risks of arthroplasty?
The potential complications/risks associated with the surgery include:
- Infection in the operated site
- Bleeding
- Formation of blood clots in lungs/legs
- Dislocation of the implanted prosthesis
- Damage to the nerves or blood vessels in the operated area
- Breaking of bone around the implanted prosthesis
- Need for further surgery
- Risks of general anaesthesia such as confusion, lung infection, and stroke.
When to follow up with your doctor after an arthroplasty?
Your surgeon will provide you with a schedule for follow-up appointments before discharging you from the hospital. During the follow-up appointments, your stitches will be removed, and the surgeon will examine the operated site.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- Stanford Healthcare [Internet]. University of Stanford. California. US; Arthroplasty (Total Joint Replacement Surgery)
- Orthoinfo [internet]. American Academy of Orthopaedic Surgeons. Rosemont. IL. US; Hip Resurfacing
- American Association of Hip and Knee Surgeons [Internet]. Illinois. US; Full vs. Partial Knee Replacement: What's the difference?
- Lucile Packard Children's Hospital Stanford [Internet]. Stanford Children's Health. Stanford University. California. US; Anatomy of a Joint
- Johns Hopkins Medicine [Internet]. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System; Arthroplasty
- National Health Service [Internet]. UK; Knee replacement
- Hsu H, Siwiec RM. Knee Arthroplasty. [Updated 2020 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Varacallo M, Luo TD, Johanson NA. Total Hip Arthroplasty Techniques. [Updated 2020 Jul 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Eichinger JK, Galvin JW. Management of complications after total shoulder arthroplasty. Curr Rev Musculoskelet Med. 2015;8(1):83–91. PMID: 25672497.
- Hernandez A, Sherwood ER. Anesthesiology principles, pain management, and conscious sedation. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 14
- Cleveland Clinic [Internet]. Ohio. US; A Patient’s Guide to Total Joint Replacement and Complete Care