Summary
Lung transplant is a surgery that aims to replace a diseased or affected lung with another healthy human lung. This surgery is recommended for individuals with severe, life-threatening lung diseases and a reduced life expectancy without the surgery (12-24 months). You need to undergo a detailed pre-operative assessment to confirm your eligibility for the surgery. Once eligible, you will have to enrol in the waiting list until the availability of a suitable donor. When a suitable donor is available, the hospital will notify you and you have to arrive at the hospital as soon as possible. You need to be hospitalised for about seven to 10 days after the surgery. You may take up to three to six months to completely recover from the surgery.
- What is lung transplant?
- Why is lung transplant recommended?
- Who can and cannot get lung transplant?
- What preparations are needed before lung transplant?
- How is lung transplant done?
- How to care for yourself after lung transplant surgery?
- What are the possible complications/risks of lung transplant?
- When to follow up with your doctor after a lung transplant?
What is lung transplant?
Lung transplant is a surgery where the surgeon replaces a diseased/affected lung with a healthy, suitable lung from a human donor.
This surgery is performed in individuals with severe, life-threatening lung diseases who do not respond to other treatments or if the life expectancy of the individual is 12-24 months without this surgery. The four types of lung transplant procedures are as follows:
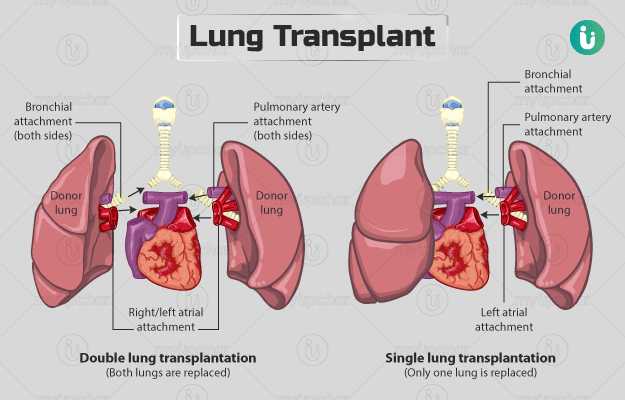
- Single lung: Only one lung is replaced.
- Double lung: Both lungs are replaced.
- Bilateral sequential: Both lungs are replaced, one at a time.
- Heart-lung transplant: Both the lungs, as well as the heart, are replaced with the heart and lung of a single donor.
The organs (lungs and heart) for transplant are usually obtained from deceased donors who were healthy and non-smoking individuals (cadaveric transplant). However, in some cases, a healthy living individual donates a portion (lobes) of their lung - lobectomy. Such transplant is referred to as living transplant, and these individuals continue to live a healthy life even after donating a part (lobes) of their lung.
Why is lung transplant recommended?
The surgeon may recommend this surgery to treat any of the following conditions in a severe stage when other treatments have not produced any favourable outcomes:
-
Cystic fibrosis: Symptoms of this inherited disease are:
- Pain in the joints and muscles
- Jaundice
- Mucus- or blood-containing cough
- Chronic obstructive pulmonary disease: Symptoms of this disease are:
- Tightness in chest
- Respiratory infections
- Continual cough with a lot of mucus
- Idiopathic pulmonary fibrosis: Symptoms of this condition are:
- Pain in the joints and muscles
- Shallow and rapid breathing
- Moderate and unexpected weight loss
- Pulmonary hypertension: Symptoms of the condition are:
- Alpha-1 antitrypsin deficiency: Symptoms of this protein deficiency include:
- Repeated infections in the lung
- Chronic cough
- Fatigue
- Bronchiectasis: Symptoms of this condition are:
- Pain in chest
- Cough for a prolonged period (months or years)
- Thickening of the tips of fingers and toes
- Sarcoidosis: General symptoms of this condition are:
- Fever
- Depression
- Loss of weight
Wheezing and shortness of breath are commonly observed symptoms in all the lung diseases.
In cases when an individual has a heart condition and breathing problems that are life-threatening, e.g., cystic fibrosis or Eisenmenger' s syndrome, a heart-lung transplant is recommended.
If you are tired of dieting and exercising and are not able to lose weight, then use myUpchar Ayurveda Medarodh Fat Burner Capsule, it has no side effects, order it today and avail the benefits.
Who can and cannot get lung transplant?
The surgeon may consider you ineligible for the surgery if:
- You are more than 50 years (ineligible for a heart-lung transplant).
- You are more than 65 years (ineligible for a double lung transplant and in some cases, for single lung transplant too).
- You are either underweight or overweight.
- Your lung disease is at an advanced stage.
- Your other vital organs (heart, kidneys and liver) do not function properly.
- The surgeon feels that you do not comply with the advice and restrictions imposed on you, such as stopping smoking, attending scheduled hospital visits and taking the prescribed medicines
- You have an infection.
- You recently suffered from cancer, and the surgeon suspects that cancer can spread to the new lung.
- You suffer from psychological or social problems such as serious mental health conditions or drug addiction.
What preparations are needed before lung transplant?
As part of the pre-operative assessment, a series of medical tests will be performed to ensure your eligibility for the transplant. These tests help to ensure the effective working of other vital organs of the body such as heart, kidney and liver after lung transplant. Generally, the assessment requires a hospital stay of about three days. Some of the tests that may be performed are:
- Blood test
- Chest x-ray
- Electrocardiogram or ECG (a test to record or measure the electrical activity of the heart)
- Echocardiogram (a test to check the ability of the heart to pump blood effectively)
- Angiogram (a type of x-ray that checks the blood flow in the lung’s blood vessels)
If you are considered eligible for the lung transplant, the hospital will register you on the National Organ and Tissue Transplant Organisation portal. When a suitable donor is available, then you will have to arrive at the hospital immediately, usually within six to eight hours.
During your waiting period for a new lung, the surgery may ask you to:
- Practice special exercises that your doctor taught you
- Avoid drinking alcohol and smoking
- Follow the recommended diet and maintain a suitable weight
- Regularly attend appointments with your surgeon and other doctors looking after your transplant
- Share the list of all the medicines you are taking (previous or current), including supplements, herbs, prescription and over-the-counter medicines
- Take medicines as prescribed and directed by the surgeon
As soon as the hospital notifies you of the availability of a lung for transplant, you should arrive at the hospital at the earliest. To make sure that the surgery can be done at the earliest, try to avoid eating or drinking anything soon after you get information about the availability of the lung (fasting is required for at least 8 hours for a lung transplant with living donor and a lung cannot stay stable for long outside the body for long). If the surgeon asks you to take any medicines, then do so with a small sip of water.
How is lung transplant done?
Upon your arrival at the hospital, the hospital staff will ask you to sign a consent form, allowing them to perform the surgery. You will then be asked to put on the hospital gown and urinate to empty your bladder. You may also be asked to remove accessories such as jewellery, nail polish, makeup, dentures, and eyeglasses or contact lenses. Inform the medical staff if you have any signs of infection, such as fever, cold or sore throat. The surgery usually involves the following steps:
- The surgeon will insert an intravenous line into your hand or arm to provide you with fluids and a thin, flexible tube either into your wrist, neck, groin or under your collarbone to monitor your blood pressure and heart activity and to collect blood for testing.
- You will be asked to position yourself on the operating table based on which lung needs to be removed. For a single lung transplant, you will have to lie on the side opposite to the lung to be removed, whereas for a bilateral sequential lung transplant, you will have to lie on your back. Your arm will be kept above your head.
- An anesthesiologist will administer general anaesthesia (to make you sleep during the procedure).
- A breathing tube will be placed down your throat, which will be connected to a ventilator (breathing machine).
- The surgeon or the medical team will put another flexible tube (catheter) into your bladder to drain out urine.
- Then, he/she will shave off your hair on the area to be operated, and clean the area with an antiseptic solution.
- For a single lung transplant, the surgeon will make a horizontal incision on the side of your chest from where the lung is to be replaced. For a bilateral sequential lung transplant, the surgeon will introduce a horizontal incision below your breast/chest to access both the lungs or a horizontal incision between your breasts. For a heart-lung transplant, a clamshell-shaped incision will be made on your chest through which the heart and lung are replaced.
- The surgeon will connect your body to a heart-lung machine, which will work as your lungs and heart during the surgery.
- He/she will then remove the diseased lung and replace it with the donor’s lung.
- Next, the surgeon will attach the blood vessels and airways of the donor’s lung to your body.
- Once that is done, he/she will close the incisions with surgical staples or stitches and cover it with a dressing.
- The surgeon may insert tubes into your chest to remove fluid, blood and air from your chest cavity. This action helps the transplanted lung to expand freely.
- He/she may also insert a thin tube into your back to deliver medicines for the pain.
After the surgery, the hospital staff will shift you to the intensive care unit where your vital signs will be watched closely. You may need to be hospitalised for about seven to eight days. You can expect the following events during this period:
- You will be on ventilator support for up to a few hours to a few days after the procedure until you can breathe freely.
- The medical team will insert a thin tube into your stomach via your nose to remove any air that you may swallow. This tube will be in place until the normal functioning of your digestive system. You will not be able to eat/drink during this period. The catheter in your bladder will also be there until you can urinate by yourself.
- You may be allowed to start a liquid diet once the breathing tube and stomach tube are removed. Your diet will slowly be moved to solid foods depending on how well you tolerate it.
- The medical staff will teach you certain breathing exercises. They may also begin physical therapy.
- You will be administered antirejection medicines (medicines to suppress the immune system) to keep the lung from being rejected by your immune system.
- The delivery of pain medicines will be continued via the tube inserted in your back or through an IV route.
How to care for yourself after lung transplant surgery?
The surgeon may advise the following measures for self-care at home:
- Refrain from lifting, pulling and pushing heavy objects for the initial six weeks post-surgery.
- You will be encouraged to participate in rehabilitation programmes, which include certain exercises that will help you in regaining strength.
- Consult the surgeon before resuming driving. You may be allowed to drive four to six weeks after surgery until the complete healing of your wounds.
- Your recovery period after which you can resume work depends on the type of work you do. It usually takes around three months until recovery.
- The surgeon will prescribe a few anti-rejection medicines that may cause side effects such as:
The surgeon will regularly change the dose of antirejection medicines over months to find a suitable dose that suppresses your immune system (to avoid rejection) and produces minimal side effects. You should not stop taking the antirejection drugs even if the side effects become troublesome, instead, it is best to talk to your doctor about it. Meanwhile, keep the following things in mind:
- Infection is one of the main complications after the surgery. Therefore, avoid contact with people with infections since it could severely affect you.
- Keep the surgical area clean and dry. Adhere to the surgeon’s special instructions for bathing.
- Practice good hygiene habits. Shower regularly and wash your towels and linens frequently.
- Wash your hands frequently, especially after meals and going to the toilet.
- Be extra careful in preventing yourself from any cuts on the skin. If any object cuts or grazes your skin, then clean the area with warm water and use a sterile bandage or dressing to cover it.
- Keep yourself up-to-date with all the vaccines relevant to you.
Lung transplant helps in the management of life-threatening lung diseases. The benefits of the surgery include better exercise endurance and quality of life and extended lifespan.
When to see the doctor?
Rejection and infection are the two main complications after surgery. Hence, you should look for these signs during the recovery period. You should inform the hospital immediately if you experience any of the following rejection symptoms:
- Decreased breathing
- Fever
- Coughing
- Congestion in chest
- Pain around the new lung
- A feeling of uneasiness
Similarly, contact the surgeon if you observe any of the following signs of infection:
- High temperature
- Aching muscles
- Headache
What are the possible complications/risks of lung transplant?
The risks associated with the surgery include:
- Rejection of the new lung right away or over a period
- Formation of blood clots in the body
- Reaction to antirejection and other medicines given after surgery, such as:
- Increase in the risk of infections
- Damage to organs such as kidneys and liver
- Thinning of bones
- Diabetes
- Increased levels of cholesterol
- Damage to the new airway and blood vessels at the site of attachment
- The new lung may stop functioning
When to follow up with your doctor after a lung transplant?
The hospital staff will provide you with a schedule for follow-up visits before discharge. Follow-up visits will be needed for the following purposes:
- To remove staples or sutures from the incision site
- For medical and imaging tests such as blood tests, chest x-ray, biopsy, bronchoscopy and pulmonary function tests.
- For rehabilitation programmes.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- Johns Hopkins Medicine [Internet]. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System; Lung transplant
- UCSF Department of Surgery [internet]. University of California San Francisco. California. U.S.A.; Lung Transplant
- National Heart, Lung, and Blood Institute [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Health topics
- Blatter JA, Noyes B, Sweet SC. Kendig's disorders of the respiratory tract in children. 9th ed. Philadelphia, PA: Elsevier; 2019. Chapter 67, Pediatric lung transplantation.
- Chandrashekaran S, Emtiazjoo A, Salgado JC. Textbook of critical care. 7th ed. Philadelphia, PA: Elsevier; 2017. Chapter 158, Intensive care unit management of lung transplant patients.
- Robert J. Mason, et al. Murray & Nadel's textbook of respiratory medicine. 6th ed. Philadelphia, PA: Elsevier Saunders; 2016. Chapter 106, Lung transplantation.
- Kliegman RM, Stanton BF, St. Geme JW, Schor NF. Nelson Textbook of Pediatrics. 20th ed. Philadelphia, PA: Elsevier; 2016. Chapter 443, Pediatric heart and heart-lung transplantation.
- American Lung Association [internet]. Chicago. Illinois. US; Sarcoidosis Symptoms and Diagnosis
- Harvard Health Publishing. Harvard Medical School [internet]: Harvard University; Heart-Lung Transplant
- National Health Service [internet]. UK; Preparation lung transplant
- National Organ and Tissue Transplant Organisation [Internet]. India; Allocation criteria for heart, lung and heart-lung contents
- Cleveland Clinic. [Internet]. Cleveland. Ohio. US; Lung Transplant Surgery: Procedure Details