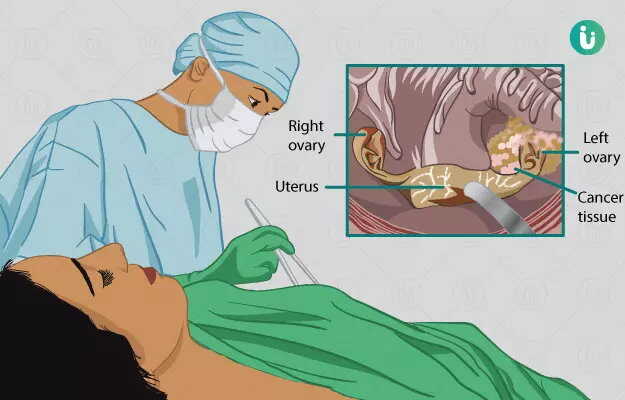
Oophorectomy is a surgical procedure where one or both ovaries are removed. It is required in pathological conditions related to the ovary where medical management has a limited role.
The surgery, if it includes removal of both ovaries, develops infertility and menopause. Hence, appropriate counselling for the patient is required before going through with the surgery. Investigations usually include blood tests and radiological tests.
The duration of the surgery and hospital stay afterwards depends upon the technique employed and the nature of the disease. Postoperative recovery varies from two to six weeks.
- What is Oophorectomy
- Why is oophorectomy done?
- When should ovary removal surgery not be done
- Preparations before the surgery
- What happens during ovary removal surgery
- Risks and outcomes of oophorectomy
- Aftercare, discharge and follow up after oophorectomy
- Takeaway
What is Oophorectomy
The ovaries are a pair of organs that form part of the internal genitalia of the female reproductive system. The ovaries primarily have two functions:
- Production of the eggs required to make a baby; and
- The production of hormones (estrogen and progesterone) that regulate the functioning of the uterus, especially in menstruation. The hormones are also responsible for maintaining bone and heart health.
Any abnormalities in the ovaries can cause issues in the two functions.
Diseases primarily concerning the fallopian tube and uterus can also affect the ovaries. When medical management fails, surgery is the treatment of choice. The removal of the ovary is known as oophorectomy.
This can be either unilateral (removing single ovary) or bilateral (removing both ovaries). Unilateral oophorectomy usually does not interfere with infertility or hormonal functioning. However, the consequence of bilateral oophorectomy is infertility and menopause (cessation of menstruation). Depending on the approach of surgery, there are three methods of oophorectomy:
- Laparotomy approach
- Laparoscopic approach
- Vaginal approach
Why is oophorectomy done?
There are numerous indications of the surgery. It is advised when medical management of the condition is unsuccessful. The indications include:
- Endometriosis: this is a condition in which cells of the inner lining of the uterus travel and grow elsewhere, such as on the ovaries
- Tumours or cysts in the ovary which are non-cancerous
- Ovarian cancer
- Tubo-ovarian abscess: an infection that presents as a pus-filled pocket involving the fallopian tube and ovary.
- Ovarian torsion: Twisting of the ovary that results in the cutting off of blood supply to the ovary. The patient will present with intense abdominal pain. This is a medical emergency.
- Ectopic pregnancy or rupture of ectopic pregnancy: when a pregnancy occurs in other parts of the reproductive tract other than the uterus (most commonly in the fallopian tubes). A ruptured ectopic pregnancy presents itself with sudden intense pain and is a medical emergency.
- Pelvic inflammatory disease is a condition that involves infection and inflammation of the entire internal reproductive system
- In certain individuals, the presence of certain genetics is a contributing factor for ovarian and breast cancer. In such people, this surgery is performed prophylactically.
When should ovary removal surgery not be done
The procedure is a major surgery. Relative contraindications for the surgery include:
- Any pre-existing conditions such as diabetes, heart disease, bone diseases. These need to be kept under control before going through with the surgery, since such conditions increase the risk of anaesthetic complications and duration of recovery post-surgery
- Active cancer with metastasis (cancer that has spread to other tissues)
- In women who wish to conceive in the future, bilateral oophorectomy is not advised unless necessary.
Preparations before the surgery
The surgery is performed by an OBG surgeon. A detailed discussion between the surgeon and the patient is done explaining the procedure, the risks of the surgery and the associated outcome. A detailed history of the patient is taken which includes the symptoms of the patient, any history of comorbidities (pre-existing conditions), menstrual history, family history and medication history. A physical examination of the patient is also done.
Counselling of the patient is important, especially if both ovaries are being removed because the consequences would result in infertility and menopause (also known as surgical menopause). If any woman wishes to conceive even after the surgery, a visit to a fertility doctor prior to the procedure is advised to store the woman's eggs for the future. Surgical menopause can result in heart and bone-related pathologies hence, treatment options for those conditions will be discussed beforehand.
Medications, if any, for any pre-existing conditions may be altered/stopped prior to the surgery as per the surgeon’s orders.
Investigations include:
- Routine blood investigations
- Routine urine tests
- Chest X-ray
- ECG
- Ultrasound of the abdomen and pelvis, to visualise and assess the ovaries
- In some cases, an MRI or CT scan of the abdomen may be required
The procedure is a major surgery and hence, the patient will require a few days of hospital stay. The patient is admitted usually a day or two before the date of the surgery, with all the necessary reports and documents. Post-admission the patient changes into the hospital gown. Preoperative instructions include:
- Continuing any medications as prescribed by the doctor for any pre-existing illness. Since the procedure is a major one, blood is already arranged and kept ready in case of major blood loss during the surgery.
- Taking consent for surgery from the patient and relatives while explaining the risks and outcomes.
- Preparing the site of surgery, viz. shaving the hair around the pelvis, abdomen and legs and taking a bath.
- Switching the diet from solid to liquids to finally intravenous fluids, so that the patient is fasting for around 8-10 hours (overnight fasting) before surgery.
- Give the patient a laxative to cleanse the bowels of faecal matter
- Due to anxiety before the surgery, the patient can be given a mild sedative prescribed by the doctor so that the patient has a restful sleep before the procedure.
A final review of the patient by the surgeon and nurse is carried out to clear the patient for the surgery. Thereafter, the patient is shifted into the operation theatre (OT).
What happens during ovary removal surgery
The patient is made to lie supine (on their back) on the operating table. A monitor is attached to keep track of the vitals (heart rate, blood pressure and oxygen saturation) of the patient. An IV cannula is inserted to administer medications during the surgery (antibiotics/ anaesthesia). A urinary catheter is inserted to prevent urine from contaminating the surgical area. The area of surgery is cleaned and the surrounding area is covered with surgical drapes. The procedure is done usually under general anaesthesia. Depending on the technique of surgery used the surgery can be undertaken in any of the following ways:
- Laparotomy: A long midline incision (cut) is made on the abdomen. This allows better access to the abdomen and is a much simpler method to remove ovaries. However, the risk of infection and duration of healing is higher as compared to the other methods
- Laparoscopic: In this method, 2 -3 minor incisions are made on the abdomen, creating ports. Through one port, a flexible camera is inserted to help visualise the internal abdomen. The other ports are used to insert special surgical tools that will remove the ovaries.
- Vaginal: The approach is usually employed when the uterus is also being removed along with the ovaries. The patient in this procedure is placed in the lithotomy position (the patient is lying on their back and the legs of the patient are spread wide when giving birth). The surgeon approaches the abdomen through the vagina and with the help of special surgical tools removes the ovaries, fallopian tubes and the uterus.
Depending on the extent to which the surgery is performed, oophorectomy can be further classified as:
- Unilateral oophorectomy: removing one ovary
- Bilateral oophorectomy: removing both ovaries
- Salpingo-oophorectomy: removing the ovary along with the fallopian tube
- Bilateral salpingo-oophorectomy: removing both ovaries and their fallopian tubes
- Hysterectomy with salpingo-oophorectomy: removing the uterus along with the fallopian tubes and ovaries.
Each procedure has its own duration, associated risks and recovery time. In cases where hysterectomy is performed, a surgical drain may also be placed which drains out excess blood and fluid from the pelvis. Once the procedure is done, the incisions are sutured (stitched) and the ovaries are sent to the pathology lab for further studies.
Risks and outcomes of oophorectomy
Although major, the surgery has considerably low risks. Some of the complications seen are:
- Excessive bleeding during the surgery
- Injury to the surrounding structures, such as the bladder and bowels
- Injury to tumours/ cysts which results in spilling of their contents into the abdomen
- Incomplete removal of the ovarian tissues results in a condition called ovarian remnant syndrome. It is characterised by chronic pelvic pain.
- Infection of the incision sites
- Excessive swelling or pain at the incision site
- In patients where both ovaries are removed, the patient becomes infertile and surgical menopause sets in immediately
Aftercare, discharge and follow up after oophorectomy
After the surgery, the patient is shifted from the OT into an observation room for a few hours before being shifted to the ward. In some cases, the patient may be kept in the ICU for overnight monitoring.
Pain is controlled via analgesics. IV antibiotics are administered to prevent infection. The urinary catheter is kept for approximately 24 hours and in some cases, maybe kept for a few days. Passage of gas indicates wearing off of anaesthesia and no bowel complications. The drain, if present, is measured daily for the amount of fluid collected; it is removed when minimal fluid is present.
Dressing at the incision site is regularly checked. Ambulation (walking) of the patient is advised as soon as the patient is able to. Diet is changed from liquid to semi-solid to normal diet over the next 12 to 24 hours. Once the patient can perform light daily activities, the patient can be discharged.
A discharge summary is prepared by the surgeon that contains relevant medications and advice on wound care. These typically include:
- Continuation of medication for pre-existing conditions, if any
- Antibiotics and analgesics to prevent infection and pain, respectively.
- Instructions on wound care and dressing hygiene are given to prevent infection at the incision site
- Advice is given on not indulging in sexual activities as well as strenuous activities such as weight lifting, cycling, etc. for a few weeks as per the surgeon’s orders
- In case of surgeries involving the removal of both the ovaries, the patient develops menopause and will be started on hormone replacement therapy.
The surgeon is to be notified if any of the following symptoms arise:
- Excessive bleeding from the wound site
- Pus discharge from the wound site
- Excessive swelling and pain at the wound site
- Difficulty in urinary or bowel habits
- Fever
- Excessive depression, hot flushes, mood swings are features when both ovaries are removed and are due to menopause.
The first follow-up occurs within a week where the sutures for the laparoscopic type of surgery is removed. The laparotomy suture removal may take some more days. The surgeon will also assess the compliance and adjustment of the patient to hormone replacement therapy if surgical menopause was achieved. Furthermore, other family planning options will be addressed and discussed over subsequent visits. Counselling to deal will the symptoms of menopause and infertility may also be advised. The wound recovery ranges from 2 to 6 weeks depending on the type of approach used.
Takeaway
Oophorectomy is a surgery where either one or both ovaries are removed (other organs of the genital tract may also be involved). The surgery is advised when medical management is ineffective. The surgery has a low risk and is sometimes life-saving. Modern techniques of surgery have reduced the post-operative recovery time. If both ovaries are removed, surgical menopause and infertility sets in which are both life-altering changes for the patient. Hence, adequate counselling for the patient is necessary pre- and post-surgery to help maintain a normal lifestyle. In addition, menopause can be managed via hormone replacement therapy and infertility can be addressed by modern assisted reproductive methods.
Find Obstetrician and Gynaecologist in cities
- Obstetrician and Gynaecologist in Bangalore
- Obstetrician and Gynaecologist in Mumbai
- Obstetrician and Gynaecologist in Ghaziabad
- Obstetrician and Gynaecologist in Chennai
- Obstetrician and Gynaecologist in Pune
- Obstetrician and Gynaecologist in Delhi
- Obstetrician and Gynaecologist in Hyderabad
- Obstetrician and Gynaecologist in New Delhi
- Obstetrician and Gynaecologist in Gwalior
- Obstetrician and Gynaecologist in Gurgaon
Surgery Cost In Your City
Doctors for Oophorectomy

Dr. Ayushi Gandhi
Obstetrics & Gynaecology
4 Years of Experience

Dr. Anjali
Obstetrics & Gynaecology
23 Years of Experience

Dr.Anuja Ojha
Obstetrics & Gynaecology
20 Years of Experience