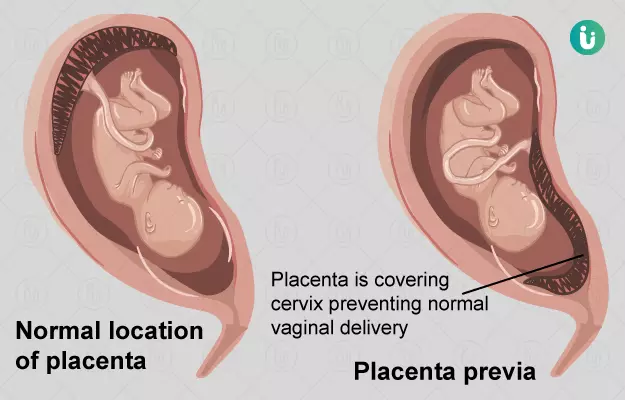
Placenta previa is a condition in which the placenta covers the cervix (which links the uterus to the vagina) marginally, partially or completely.
Here’s how this occurs: The development of the placenta begins soon after a fertilised egg gets implanted in the uterus. Usually, the blastocyst (the fertilised egg that has already taken the first steps towards becoming an embryo) gets implanted towards the top, side, front or back of the uterus. In one out 200 pregnancies, however, the blastocyst gets implanted so close to the cervix that the placenta ends up covering all or part of the cervix as it develops.
Placenta previa in the early stages of pregnancy may resolve on its own—as the uterus gets bigger to accommodate the growing baby, it may pull the placenta up and away from the cervix by the 20th week of pregnancy. If this doesn’t occur, your doctor may recommend an ultrasound during the 32nd week of pregnancy to monitor the position of the placenta. You may also be advised bed rest or at least less strenuous activity in the latter half of your pregnancy—for some women, this also means no sex during pregnancy.
Placenta previa is associated with a few complications. To begin with, women with a low lying placenta and placenta previa may experience vaginal bleeding; the use of a tampon is not recommended if your bleeding during pregnancy is due to placenta previa.
Placenta previa in the latter half of the pregnancy also increases the risk of heavy bleeding during and after labour—as the cervix effaces (becomes thinner) and dilates (opens up) during labour, it could damage the placenta and severe some of the blood vessels running from the uterus to the placenta. This is considered to be one of the major causes of death during childbirth in developing and poor countries.
Placenta previa also increases the chances of PPROM or preterm premature rupture of membranes, in which a pregnant woman’s water breaks before 37 weeks of gestation: this can increase the chances of premature labour and infections.
Placenta previa is diagnosed through an ultrasound between the 18th week of pregnancy and the 21st week of pregnancy. A low lying placenta doesn’t feel different, though women may be able to tell the difference if they experience bleeding (the blood tends to be bright red). If you are diagnosed with this condition, it is important to stay in touch with your doctor and monitor the condition.
If the condition does not resolve enough in time for the delivery, a C-section (cesarean delivery) has to be performed.