Welcome to the 25th week of pregnancy! You’re nearing the end of the second trimester, and your baby should be thriving right now. Your baby bump has not only been growing, but now that your baby is active and you can feel him or her moving, you’ll actually be able to interact with your little bundle of joy in a way.
There are no foetal ultrasounds you need to get done this week, but make sure to ask your doctor about getting your blood sugar levels and cervical strength checked. This is because gestational diabetes usually shows up between the 24th week of pregnancy and 28th week of pregnancy, and if your cervix is weak, then carrying the ever-increasing weight of your baby will become more and more difficult.
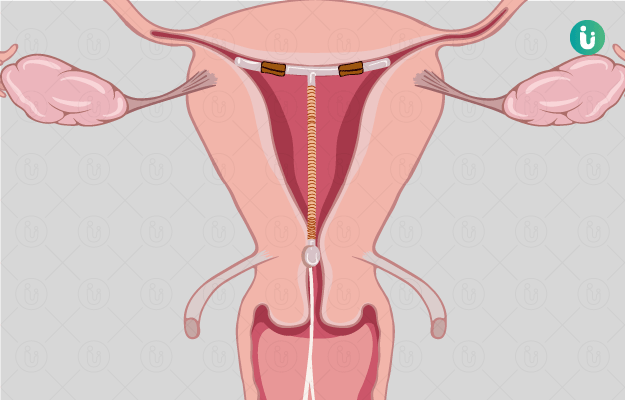
Getting a weak cervix treated is now very easy, because it involves a simple procedure called cervical cerclage, where a stitch is placed to hold the cervix until at least the 37th week of pregnancy. This is a small procedure that can reduce the risk of premature labour and keep your baby healthy. It’s usually recommended that you get this procedure done before the second trimester ends.
This apart, if you continue to follow a proper pregnancy diet and pregnancy exercise routine, you should be absolutely fine. Make sure you get enough rest and engage with others, and don’t ignore your mental health at all. Depression during pregnancy can be as harmful as postpartum depression. Here’s everything you need to know about the 25th week of pregnancy.