Summary
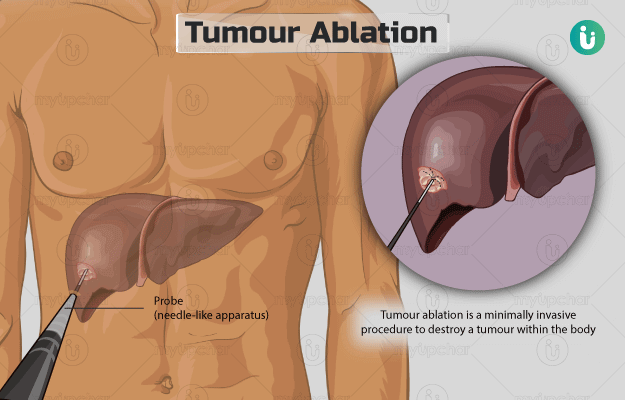
Tumour ablation is a minimally invasive procedure to destroy a tumour within the body without the need for open surgery. This is achieved by inserting a probe (needle-like apparatus) into the body through a small incision (cut) made on the skin. The probe is guided towards the tumour using imaging procedures such as ultrasound, magnetic resonance imaging (MRI), or computer tomography (CT) scan. Once the probe is within the tumour, it subjects the diseased tissue to electric current, heat, low temperature, or chemical to destroy it. The procedure lasts for around two hours, and you will be able to go home after an overnight stay at the hospital.
- What are the possible complications/risks of tumour ablation?
- When to follow up with your doctor after a tumor ablation?
- What is tumour ablation?
- Why is tumour ablation recommended?
- Who can and cannot get tumour ablation?
- What preparations are needed before tumour ablation?
- How is tumour ablation done?
- How to care for yourself after tumour ablation?
What are the possible complications/risks of tumour ablation?
The potential complications/risks associated with the procedure include:
- Infection
- Bleeding
- Collapsed lung
- The spread of the tumour to nearby organs
- Damage to nearby structures or organs
When to follow up with your doctor after a tumor ablation?
Your follow-up will be scheduled one month following the procedure wherein CT scan or MRI will be performed to help the surgeon assess the outcomes and plan further treatment if needed.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
What is tumour ablation?
Tumour ablation is a minimally invasive surgical procedure to destroy tumours in the kidney, liver, lung, bone, and other locations without removing them.
The procedure involves the insertion of a needle-like applicator (probe) into the tumour through a tiny opening in the skin. The applicator is connected to a generator that subjects the tumour to high temperature, extremely low temperatures, electric current, or concentrated alcohol to destroy tumour cells. The procedure is performed with any of the following methods:
- Radiofrequency ablation: It uses a high-frequency current produced by a radiofrequency generator to heat the needle above 60OC, and destroy the tumour.
- Microwave ablation: It uses electromagnetic energy in the microwave range, i.e., 300 MHz to 300 GHz, to produce heat and destroy tumour cells.
- Laser ablation: It uses light energy produced by neodymium:yttrium aluminium garnet lasers to heat and destroy the tumour.
- High-intensity focused ultrasound (HIFU) ablation: It uses ultrasound waves with increased intensity (compared to diagnostic ultrasound) to quickly heat and destroy the tumour.
- Irreversible electroporation (IRE) ablation: IRE uses pulses of electric current to damage the outer membrane of the tumour cells, resulting in cell death.
- Cryoablation: It uses argon gas or liquid nitrogen to subject the tumour to cold temperature and destroy the affected tissue.
- Ethanol ablation: This method involves the injection of concentrated alcohol into the tumour to destroy it.
Why is tumour ablation recommended?
Tumour ablation is recommended to destroy tumours in any part of the body that are easily accessible through the skin and of appropriate size (preferably <3 millimetres [mm]). The most common tumours treated by this procedure include
-
Lung cancer: Cancer in lungs is associated with the following symptoms:
- Shortness of breath
- Fatigue
- Loss of appetite
- Persistent infection in the lungs
- Chest pain that gets worse during coughing, deep breathing, or laughing
- Renal (kidney) cancer: Kidney cancer is associated with the following symptoms:
- Loss of appetite
- Tiredness
- Blood in urine
- Pain in the right/left side of the lower back
- Persistent fever (not caused by an infection)
- Liver cancer: Symptoms of liver cancer include:
- Nausea or vomiting
- Itching
- Abdominal pain
- Pain near the right shoulder blade
- A feeling of fullness under the ribs on the right/left side
Who can and cannot get tumour ablation?
Your surgeon will choose the method to perform tumour ablation based on the nature of your tumour, co-existing health conditions, and medical history. The factors or conditions that contraindicate different methods of tumour ablation are as follows:
- Radiofrequency and microwave ablation:
- Increased intracranial pressure
- Ascites
- Bleeding disorders
- Abnormal structure of internal organs (from previous surgery or present since birth)
- Active inflammation/infection in any organ or near the area to be operated.
- Tumours located close to the diaphragm, gallbladder, pancreas, major bile duct, digestive tract, or blood vessels.
- Laser ablation:
- Depth of tumour >6 mm
- Size of tumour between 20 mm and 50 mm
- High-intensity focused ultrasound ablation:
- Serum bilirubin level >100 μmol/L
- Thickness of subcutaneous tissue >3.5 centimetres
- Irreversible electroporation ablation:
- A history of cardiac arrhythmias
- A pacemaker in the chest
- Cryoablation: Primary liver tumours (cancer that has spread to other body parts from the liver)
- Ethanol ablation
- Coagulopathy:
- Obstructive jaundice due to the risk of main portal vein thrombosis and bile peritonitis
- Tumour under the diaphragm
- Gross ascites
- Tumour close to major blood vessels, gut, bile ducts, and stomach
What preparations are needed before tumour ablation?
You will have to visit the surgeon a few days prior to the surgery for a preoperative assessment, wherein the surgeon will ask you to share the following details:
- Your medical history
- Any allergies that you may have
- Whether you are pregnant
- A list of medicines that you take such as herbs and over-the-counter medications
In addition, you will be asked to undergo a few tests to confirm the diagnosis and ensure you are in good general health for the surgery:
- Blood test
- Urine tests
- Pregnancy test
- Biopsy (a tissue sample is taken to examine it)
- Endoscopy (a test wherein a tube is inserted inside the body to look at the tumour)
- Imaging tests such as X-ray, ultrasound, or magnetic resonance imaging (MRI)
You will also be given the following instructions to prepare for the surgery:
- Discontinue aspirin, warfarin, ibuprofen, or other blood-thinning medicines a few days before the surgery.
- Fast from the midnight prior to the surgery.
- Stop smoking if you do.
- Shower and remove all the nail polish, body piercings, and make-up before you arrive at the hospital on the scheduled day of the surgery.
- Arrange for a friend, family member, or responsible adult to drive you home after discharge from the hospital.
- Inform the surgeon if you have flu, cold, or fever on the days leading to the surgery. In such a case, your surgery may be postponed.
- You will have to sign an approval form if you agree to the procedure.
How is tumour ablation done?
After your admission to the hospital, the hospital staff will provide you with a hospital gown. They will also insert an intravenous (IV) line in your arm to provide you with essential medicines and fluids during the surgery. The procedure involves the following steps:
- The medical staff will take you to the interventional radiology surgical suite.
- You will be given a sedative or general anaesthesia. The sedative will make you drowsy; however, you will be awake during the procedure. On the other hand, general anaesthesia is a pain-numbing medicine that will put you in a deep sleep.
- You will be made to lie on an imaging table in a comfortable position depending on the location of the tumour in your body.
- Monitoring devices will be connected to your body to track your heart rate, blood pressure, blood oxygen level, and breathing during the procedure.
- Someone from the surgery team will clean and shave the area on your skin where the probe is to be inserted.
- The surgeon will make a tiny cut (incision) on the site, insert a needle through the incision and use an MRI, ultrasound, or computed tomography (CT) scan to guide the needle towards the tumour.
- Once the tumour is destroyed, the surgeon will remove the probe and cover the cut with a bandage.
- Finally, you will undergo another scan that will allow the surgeon to assess the destroyed tumour.
The procedure will last for around two hours. Although the tumour is destroyed during the procedure in a few minutes, a majority of the time is spent to guide the needle towards the correct position of the tumour. You will be moved to the observation unit after the procedure and will be discharged after an overnight stay at the hospital.
How to care for yourself after tumour ablation?
You may experience some soreness and flu-like symptoms for some days after the procedure. Your surgeon will prescribe some medicines to provide relief. Based on the location of the operated area, the surgeon will give you specific instructions to care for the area. He/she will ask you to avoid smoking, exercise regularly, and follow a healthy diet to promote quick healing.
Since the technique does not require a large cut, you will recover within a short period.
When to see the doctor?
Contact the surgeon if you experience any of the following after the discharge:
- Increased body temperature
- Increased pain, swelling, warmth, or redness near the operated site
- Loss of sensation in the surgical area
- Nausea or vomiting
Surgery Cost In Your City
Doctors for Tumour ablation

Dr. Anil Gupta
Oncology
6 Years of Experience

Dr. Akash Dhuru
Oncology
10 Years of Experience

Dr. Anil Heroor
Oncology
22 Years of Experience

Dr. Kumar Gubbala
Oncology
7 Years of Experience
References
- Knavel EM, Brace CL. Tumor ablation: common modalities and general practices. Tech Vasc Interv Radiol. 2013;16(4):192–200. PMID: 24238374.
- American Cancer Society [Internet]. Georgia. US; Ablation for liver cancer
- Johns Hopkins Medicine [Internet]. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System; Tumor Ablation
- Wray JK, Dixon B, Przkora R. Radiofrequency Ablation. [Updated 2020 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Medical Services Advisory Committee: Department of Health [Internet]. Australian Government; Final protocol to guide the assessment of microwave tissue ablation for primary and secondary liver cancer
- Cheung TT, Fan ST, Chan SC, Chok KSH, Chu FSK, Jenkins CR, et al. High-intensity focused ultrasound ablation: an effective bridging therapy for hepatocellular carcinoma patients. World J Gastroenterol. 2013 May;19(20):3083–3089. PMID: 23716988.
- Narayanan G. Irreversible electroporation. Semin Intervent Radiol. 2015 Dec;32(4):349–355. PMID: 26622097.
- Islam MN, Saha MM, Ahsan M, Mashud G. Percutaneous ethanol injection for ablation of hepatocellular carcinoma. Bang Med J (Khulna). 2010;43:12–17
- National Health Service [Internet]. UK; Having an operation (surgery)
- Hernandez A, Sherwood ER. Anesthesiology principles, pain management, and conscious sedation. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 14
- Cedars Senai [Internet]. California. US; Tumor Ablation Procedure Information
- UCLA health [Internet]. University of California. Oakland. California. US; Tumor Ablation
- Penn Medicine [Internet]. University of Pennsylvania. Pennsylvania. US; Tumor Ablation