Hemiparesis is weakness or the inability to move on one side (right or left) of the body, which makes mobility and activities of daily living difficult. Problems that arise from one-sided impairment of arms, hands, face, chest, legs or feet can cause loss of balance (making the person stumble or fall), difficulty walking, slurring of speech, inability to grasp objects, decreased precision of movements, lack of coordination and muscle fatigue. However, the degree of weakness is variable and can range from mild to complete paralysis, as with hemiplegia. The motor symptoms and parts of the body impacted vary based on the part of the central nervous system (brain and spinal cord) that has taken a hit. Therefore, motor symptoms can occur in conjunction with other signs and symptoms. Hemiparesis motor symptoms can either occur on the same side as the brain injury, in which case it’s called ipsilateral hemiparesis or on the opposite side (i.e. right-sided injury producing left-sided weakness), resulting in contralateral hemiparesis.
The most common cause of hemiparesis is stroke. Strokes can occur due to various causes and are broadly of three types – ischaemic, haemorrhagic or transient ischaemic attacks. Ischaemic strokes can, in turn, be thrombotic, in which a thrombus or blood clot is erroneously formed in a major blood vessel, cutting off its blood flow, or embolic, wherein a previously formed blood clot, or embolus, in another part of the body is dislodged and travels through the circulatory system to lodge in an important artery. Irrespective of the cause of stroke, the blood and oxygen supply is cut off to the part of the brain or spinal cord tract supplied by the affected artery. This causes nervous tissue to undergo necrosis and die. As the impacted part of the central nervous system becomes dysfunctional, the motor and sensory activity controlled by it in the body is affected. The severity of the symptoms depends on the size, part and extent to which the brain or spinal cord are affected. Besides motor symptoms, sensory symptoms involving speech, smell, sight, vision, taste and touch are possible.

 Doctors for Hemiparesis
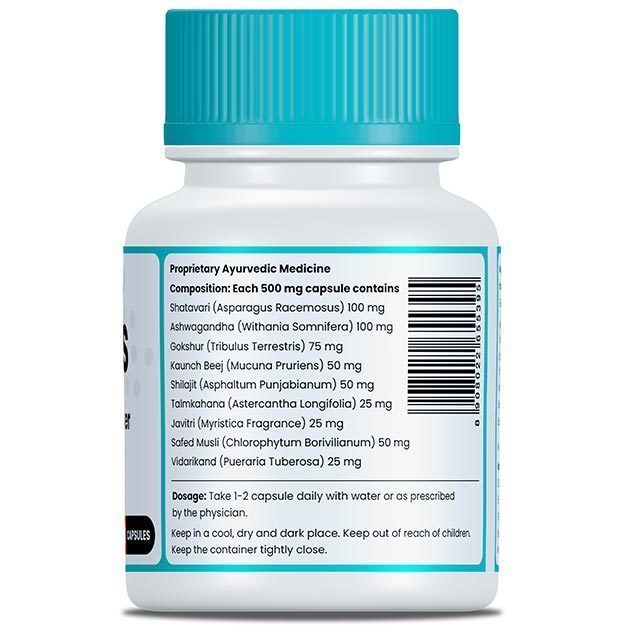
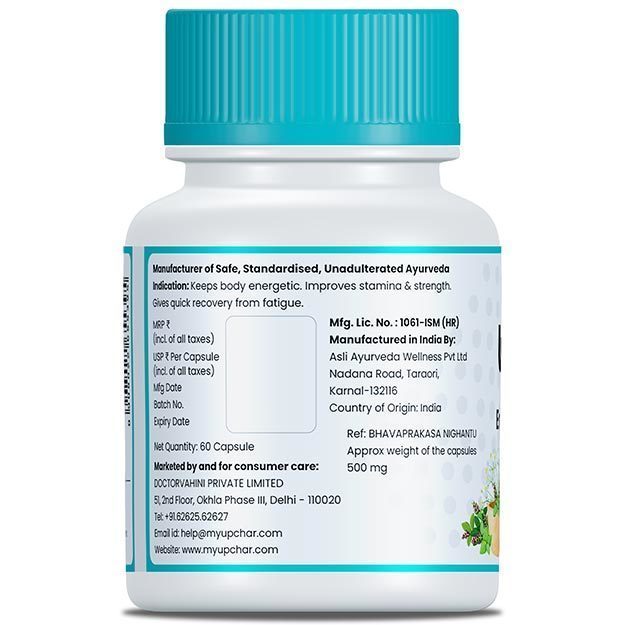
Doctors for Hemiparesis  OTC Medicines for Hemiparesis
OTC Medicines for Hemiparesis