Summary
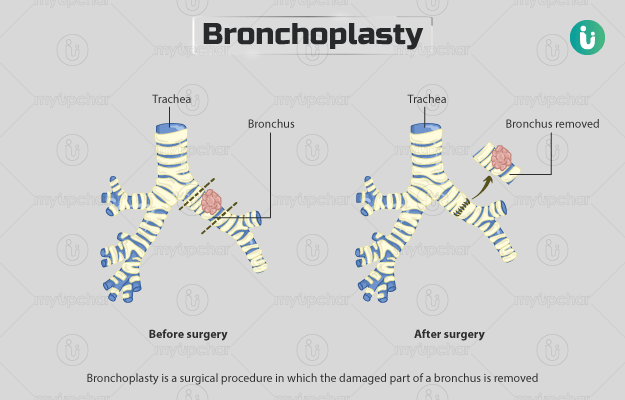
Bronchoplasty is a surgical procedure in which the damaged part of a bronchus (airway in the respiratory tract) is removed. The damage may be due to the presence of inflammatory stenosis, tumours or trauma. The surgery is contraindicated if the tumour has metastasised, there is active inflammation, or you are taking high doses of corticosteroids or radiation therapy.
Before the surgery, you will need to undergo different tests, including chest X-ray, pulmonary function tests, and ultrasound.
After the surgery, you will need pain medication and will be asked to perform breathing exercises. You will stay in the hospital for about two to five days. Your recovery will include performing lung exercises, stretching, and walking around. Certain activities like weight lifting and driving will not be permitted for a while after the surgery. A follow-up visit will be scheduled two weeks after the surgery to remove the stitches and perform various tests to check healing.
- What is bronchoplasty?
- Why is bronchoplasty recommended?
- Who can and cannot get a bronchoplasty?
- What preparations are needed before bronchoplasty?
- How is bronchoplasty done?
- How to care for yourself after bronchoplasty?
- What are the possible complications/risks of bronchoplasty?
- When to follow up with your doctor after a bronchoplasty?
What is bronchoplasty?
Bronchoplasty is the surgery performed to treat lesions in the bronchus (part of airways in the respiratory system) that may have been caused by trauma, tumours or inflammation.
The respiratory system involves various parts including lungs, airways, and blood vessels which help you breathe. The airways carry air to your lungs which then exchange oxygen for carbon dioxide from blood.
The air taken in through nose or mouth passes through the throat (pharynx) into the windpipe (trachea). The trachea splits into the bronchi, the pipes that connect it to the lungs, thus carrying the air into the lungs. Bronchi further divide into small tubes known as bronchioles in both the lungs. The latter lead to alveoli, the tiny sacs in which the oxygen from the air is absorbed by the body and the carbon dioxide is released. On the outside, lungs are surrounded by thin coverings called pleura and finally, ribs surround the lungs and heart, forming a protective cage.
Lesions or tumuors in the bronchus would thus affect the airways and cause difficulty breathing and other problems including chest pain and cough. A bronchoplasty provides relief from all these symptoms
Why is bronchoplasty recommended?
A bronchoplasty is performed in the following conditions:
- Stenosis of the bronchi (narrowing) due to inflammation
- Tumours in the airways
- Damage to the bronchi due to trauma
The symptoms of bronchial stenosis include:
- Coughing
- Fatigue
- Wheezing
- Shortness of breath
- Frequent infections in the lower respiratory tract
- A slight bluish colour of the skin
Airway tumours may cause the following symptoms:
- Cough
- Chest pain
- Wheezing
- Coughing blood
- Shortness of breath
- Recurring pneumonia
- Lung collapse due to obstruction
Who can and cannot get a bronchoplasty?
A bronchoplasty is relatively contraindicated (surgery can be performed but with caution) in the following cases:
- People who are on high doses of corticosteroids
- Exposure to high doses of radiation
- Active inflammation of the bronchi
- Metastasis (spread) of the tumour to the pleura
What preparations are needed before bronchoplasty?
The following preparations are needed before bronchoplasty:
- Your doctor will conduct a physical examination and ask you to undergo certain tests before the surgery, including :
- Blood tests
- Pulmonary function tests (to determine the amount of oxygen in your body)
- Bronchoscopy (use of an endoscope [a tube with a camera at one end] to view the internal tissues of the airways)
- Chest X-ray
- Magnetic resonance imaging (MRI) of the brain
- Computed tomography (CT) scan of the upper abdominal region and chest
- Ultrasound of the upper abdomen
- Bone scintigraphy (an imaging technique of the bones)
- Pulmonary angiogram (an imaging technique to view the blood vessels of the lungs)
- You will have to share the following details with the surgeon:
- Your doctor will ask you to stop taking aspirin, ibuprofen, warfarin, or other blood-thinning medicines before the surgery.
- You will be asked to discontinue smoking.
- You will need to fast from midnight before the surgery.
- Make sure to arrange for a responsible adult, friend, or family member to take you home after your discharge from the hospital.
- If you agree to the procedure, the medical staff will ask you to sign a consent form.
How is bronchoplasty done?
Once you reach the hospital, you will have to take your clothes off and wear a hospital gown. The hospital staff will insert an intravenous line (IV) in your arm to provide medication and fluids during the surgery. You will have to wear special stockings or take medicines to prevent the formation of blood clots in your legs. Antibiotics will be given to you to prevent any infection.
After this, you will be taken to the operation theatre and placed on an operating table. You will be attached to different devices to measure your vitals (heart rate, oxygen levels, and pulse). General anaesthesia will be administered to make you fall asleep. Once you are unconscious, a catheter (tube) will be introduced into the bladder to remove urine.
The surgeon will perform the following steps for the surgery:
- You will be asked to lie on your side, and the surgeon will make an incision (cut) between the fourth and fifth ribs or fifth and sixth ribs.
- He/she will check your chest area for any contraindications to the surgery.
- Then, the surgeon will cut off the affected region of your airway. This will be sent to the laboratory to determine whether the tissue around the affected airway (margins) is healthy.
- Thereafter, the surgeon will join the two ends of your airways with the help of sutures (anastomosis) and check the reconstructed airway for any air leaks.
- The surgeon will put drainage tubes inside your chest to remove the accumulated fluid.
- Finally, he/she will close the cut with stitches.
The surgery lasts for about six hours. Once the surgery is complete, the medical staff will move you to a recovery room or intensive care unit.
You will be initially given pain medication through the IV catheter after the surgery. The day after the surgery, you will be given medicines by mouth. Your blood pressure, heart and breathing rate will be under observation. The drainage from the drain tube will be measured, and the tube will be removed before your discharge. The medical staff will teach you how to use an incentive spirometer (a device that helps in exercising the lungs) and take deep breaths through the day. They will also help you move out of the bed and walk around a few times each day. The catheter will be removed when you wake up, and you may use the washroom as required.
You will be discharged from the hospital in about two to five days.
How to care for yourself after bronchoplasty?
Some of the ways to care for yourself include:
- Incision care:
- You can keep the incision uncovered and have a bath daily.
- Do not soak in the bathtub or hot tub for at least about two to three weeks.
- Do not rub any creams or ointments at the wound site.
- Check the surgical site daily for any complications.
- Pain medication:
- Take the prescribed pain medication as advised by the doctor.
- Place a hot water bag on the chest if you feel any stiffness. Take care to not burn yourself.
- Activities:
- Perform stretching exercises as demonstrated by your healthcare provider daily.
- You should also walk and move around at least twice or thrice a day. Slowly increase the duration of your walking.
- Keep on using the spirometer to perform breathing exercises. You should use this every hour or two and make a note of it.
- Women may prefer wearing a supportive or sports bra for comfort.
- Do not lift any heavy weights for about one to three months as directed by your doctor.
- Diet:
- A balanced meal with increased protein intake will help in healing better.
- You may also take multivitamin supplements.
- Increase your fibre intake and drink eight to 10 glasses of fluids every day to help in resuming normal bowel functions.
- Driving: Avoid driving for at least six to eight weeks after the surgery.
- Work: Your surgeon will tell you when you can resume work at your first follow-up. It may take at least a month or more before you start working again.
When to see the doctor?
See the doctor after the surgery if you have any of the following symptoms:
What are the possible complications/risks of bronchoplasty?
The surgery carries the following risks:
- Fistula (channels) between the bronchus and blood vessels or pleura
- Pneumonia
- Arrhythmia
- Sputum retention
- Air leakage from the anastomosis
- Collapse of a part of or whole lung
- Acute respiratory distress syndrome (accumulation of fluid in the lungs)
- Pus collection in the pleural cavity
- Block in the pulmonary arteries
- Complications due to general anaesthesia, including heart attack, infection in the lungs, stroke, allergic reaction, etc.
When to follow up with your doctor after a bronchoplasty?
A follow-up will take place two weeks after the surgery, in which the doctor will remove your stitches, perform a bronchoscopy, chest X-ray, and CT scan. Another follow-up will be scheduled after about three to six months, at which another bronchoscopy will be performed to assess healing.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
Doctors for Bronchoplasty

Dr. Devesh Kanoongo
Pulmonology
18 Years of Experience

Dr Viresh Mariholannanavar
Pulmonology
2 Years of Experience

Dr Shubham Mishra
Pulmonology
1 Years of Experience

Dr. Deepak Kumar
Pulmonology
10 Years of Experience
References
- Maniwa Y. Surgical treatment of airway disease. J Thorac Dis. 2016 Jan;8(1):E78–E82. PMID: 26904257.
- Cleveland Clinic [Internet]. Ohio. US; Respiratory System
- Northwestern Medicine [Internet]. Illinois. US; Symptoms of Tracheal and Bronchial Stenosis
- Stevic R, Milenkovic B. Tracheobrinchial tumors. J Thorac Dis. 2016 Nov;8(11):3401–3413. PMID: 28066620.
- Grillo HC. Surgery of the trachea and bronchi. Hamilton: Decker Inc; 2004. Chapter 30: main and lobar bronchoplasty; p. 619-630. PMCID: PMC1570594.
- Sugarbaker DJ, Bueno R, Colson YL, Jaklitsch MT, Krasna MJ, Mentzer SJ, et al. Adult chest surgery. 2nd ed. New York: Mcgraw-Hill; 2015. Chapter 75: sleeve resection/bronchoplasty for lung cancer; p. 611-619
- American College of Surgeons [Internet]. Illinois. US; Your lung operation booklet
- The American College of Obstetricians and Gynecologists [Internet]. Washington DC. US; Preparing for Surgery
- American Academy of Family Physicians [Internet]. Kansas. US; Caring for Your Incision After Surgery
- UT Health San Antonio [Internet]. Texas. US; Post-Surgery Care
- Guy's and St. Thomas' Hospital: NHS Foundation Trust [Internet]. National Health Service. UK; Recovery after lung surgery