Summary
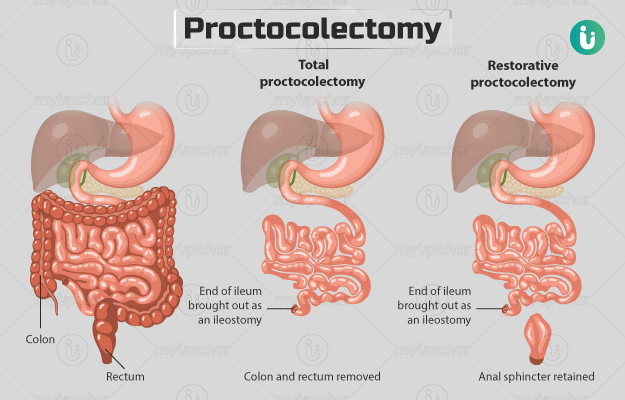
Proctocolectomy is a surgery in which the colon and rectum are removed. The colon, rectum and anus are parts of the large intestine that serves in the elimination of faeces. In conditions such as cancer and inflammatory bowel disease, these organs become diseased and may need to be removed. Proctocolectomy can be total (removal of colon, rectum, and anus) or restorative (the colon and rectum are removed, and anus is preserved). After removal of the organs, an opening may be made on the abdomen (ileostomy) through which the waste is collected.
- What is proctocolectomy?
- Why is proctocolectomy recommended?
- Who can and cannot get proctocolectomy?
- What preparations are needed before proctocolectomy?
- How is proctocolectomy done?
- How to care for yourself after proctocolectomy?
- What are the possible complications/risks of proctocolectomy?
- When to follow up with your doctor after a proctocolectomy?
What is proctocolectomy?
Proctocolectomy is performed to remove the colon and rectum (which connects the colon to the anal canal). The colon, rectum, and anal canal are parts of the large intestine, which is a long (1.5 metres) muscular tube that begins where the ileum (end of the small intestine) enters the colon and ends at the anus. Before the anus is the anal canal and rectum respectively. These are covered on the outside by the anal sphincters that help you control defecation.
The large intestine does not participate in digestion. The function of the large intestine includes holding and elimination of the waste generated after digestion (faeces) and the absorption of electrolytes and water.
Proctocolectomy may be followed by ileostomy (pouch surgery), an additional surgical procedure, to restore the waste management and elimination processes of the body.
Two types of proctocolectomy are done as follows:
- Total proctocolectomy: The colon, rectum and anus are removed.
- Restorative proctocolectomy: The colon and rectum are removed but the anus is preserved.
A proctocolectomy may be done as an open surgery (surgery is done through a longer cut on the abdomen) or laparoscopic surgery (surgery is done through several, small incisions on the abdomen).
Why is proctocolectomy recommended?
The doctor may recommend proctocolectomy if you have:
- Inflammatory bowel diseases (IBDs) such as ulcerative colitis or Crohn’s disease (characterised by ulcers and stomach pain) that do not subside with medicines
- Complications of a disease, e.g., strictures (narrowing of the intestinal canal) and fistula (an abnormal connection between the intestine and another organ) in Crohn’s disease
- Complications from earlier medical treatments
- Conversion of normal cells to cancerous cells, especially in the rectum
- Signs of IBD outside the intestines
- Ulcerative colitis that presents as pancolitis
- Synchronous multiple cancers
Restorative proctocolectomy is always desirable, but total proctocolectomy is sometimes advised in the following cases:
- Crohn’s disease with rectal inclusion
- Rectal cancer, especially at the anal end of the rectum that requires chemoradiation
- Poor continence
Who can and cannot get proctocolectomy?
Proctocolectomy is contraindicated in the following conditions:
- People with active perianal (area around the anus) infections.
- Individuals who wish to avoid the risk of sexual dysfunction caused by a proctocolectomy
- Women who want to avoid infertility caused by this surgery.
- Restorative proctocolectomy is not indicated in individuals with toxic megacolon and fulminant colitis.
- Restorative proctocolectomy is not recommended for the elderly and those who need special care or have a weak anal sphincter (muscle that controls the opening and closing of the anus).
- Total proctocolectomy is not recommended for people who wish to retain the anal sphincter.
What preparations are needed before proctocolectomy?
Preparations necessary before a proctocolectomy include:
- Blood tests, including complete blood count, electrolytes test, albumin test, or prealbumin test.
- Colonoscopy with a biopsy and CT
- Imaging tests like chest X-ray, ECG, and CT.
- Pregnancy test
- You will need to give your consent (by signing a consent form) for the procedure.
- Inform your doctor before surgery if you have conditions that affect the recovery and outcome of surgery, e.g., hypertension, diabetes, heart diseases and lung problems.
- You may require laxatives, clear liquids intake (broth, clear juice, or water), and enemas for a few days before the surgery to clean your bowel.
- A consultation with an enterostomal therapist will be scheduled to educate you about the ileostomy procedure.
- To prevent blood clots during surgery, you will daily receive heparin.
- You will be advised to fast after midnight the night before your surgery. You may take your medications with a small amount of water.
- You may be asked to stop blood thinner medicines a few days before the surgery. Medications for IBD will be continued until surgery. Medications that suppress the immune system will be discontinued after the surgery.
- Avoid smoking before surgery to prevent delayed healing.
How is proctocolectomy done?
On the day of the surgery:
- About an hour before surgery, you will receive antibiotics intravenously (through a vein).
- The doctor will place an orogastric tube (a tube is passed through the mouth into the stomach).
- A urinary catheter will also be placed during surgery to monitor urine output.
- The surgery is performed under general anaesthesia (medicine that makes you fall asleep during the procedure).
The two surgical approaches to proctocolectomy include:
Open proctocolectomy: The procedure is performed by two surgeons operating at the abdomen and perineal (near the anal opening) regions at the same time.
- A surgeon will open your abdomen along the midline. He/she will study your liver and gall bladder for gallstone or spread of cancer, the small intestine for Crohn’s disease, and the colon for a fistula or mass.
- The surgeon will then separate your colon from the other structures – right colon-caecum and ascending colon are separated from the duodenum (part of the small intestine below); he/she will free your colon from the omentum (the tissue that stretches over the abdomen) and hepatic flexure (the right-angle bend between the ascending and transverse colon). The sigmoid and descending colon will be freed from the surrounding tissues; the last part of the ileum will be separated from the colon, and the colon will be taken out from the opening.
- The surgeon will make sure to not injury the nerves and arteries in the region as they supply to essential urinary and reproductive organs.
- Next. the surgeon will free your rectum from the surrounding tissue and ligaments. Organs like the bladder in males and the bladder, uterus, and vagina in females are carefully moved aside as the rectum is freed from the connecting muscle and tissue up to the anorectal ring (muscular structure at the joining of the anal canal and rectum). The surgeon will cut the rectum circumferentially and remove it through an incision on your perineum (the region around the anal opening).
- The perineum may need to be dissected in case of low rectal cancers to remove the anal sphincter as well.
- Finally, the surgeon will close your abdominal incisions and place a drain to collect any released fluid, while the perineal opening will be sutured in layers.
Laparoscopic proctocolectomy: In a laparoscopic surgery, the surgery is done through a few small incisions on the abdomen.
- The surgeon will first make a small incision on your abdomen, and through it, fill your abdomen with carbon dioxide gas.
- He/she will make 4-5 small more incisions on your abdomen. Through one opening, the surgeon will insert a laparoscope (camera) to help him see the inside of your abdomen on a computer screen. More surgical instruments will be inserted through the other incisions.
- The laparoscopic approach follows three steps – freeing the left colon, followed by the right colon, and then the rectum. The skin is then sutured together and a drain placed. The pelvic floor is closed in layers.
Depending on how much of the area is removed, the two types of proctocolectomy are:
- Total proctocolectomy with ileostomy (Brooke’s or permanent ileostomy): In this surgery, the anus is removed along with the colon and rectum. A small opening, called a stoma, is made in the abdomen, to which the ileum is attached. The waste in the bowels passes through the ileum and is released from the stoma. It will then be collected in a pouch attached outside the body and can be emptied as necessary.
- Restorative proctocolectomy (ileal pouch anal anastomosis): In this procedure, the diseased tissue is removed. The colon is removed and the rectum is cut at the junction of the rectum and anal canal and removed; however, the anal sphincter is preserved. The end of the ileum is joined to the remainder of the anal canal with creation of an ileal pouch to collect the waste until it is excreted. Based on its shape, the ileal pouch can be J-pouch, K-pouch, or S-pouch.
Post-surgical care:
- After the surgery, the orogastric tube will be removed.
- You will be given medications to relieve pain.
- The first day after the procedure, you will be allowed to have clear fluids in limited quantities only.
- The next day, unrestricted clear fluids will be allowed. On the same day or the next, your healthcare practitioner will make a diet plan for you to suit the ileostomy, i.e., low in fibre with thickening snacks based on your ability to withstand them.
- The medicines for pain will be stopped when solid food is accepted by the body, and the catheter will be discontinued at this stage.
- You will be trained to help pass waste from the new opening in the abdomen into a bag (ostomy) will start a day after surgery.
- You will be discharged from the hospital when your oral intake is 2,000 ml, and the output through the abdominal opening is less than 1,000 mL.
- In case of open proctocolectomy, the staples on the skin will be removed and Steri-Strips (thin adhesive bandages) will be placed at the time of discharge (around six to eight days later).
How to care for yourself after proctocolectomy?
You can expect the following after surgery:
- If the rectum or anus have not been removed, you may have the sensation of moving your bowels. You may leak mucous or stool in the first few weeks.
- If the rectum is removed, the area may feel tender because of the stitches.
You can take the following care at home:
Medications:
- You will be advised to take loperamide before meals and at bedtime to prevent dehydration.
- Take all your pain medications as prescribed by the doctor.
Activity:
- Sudden jerks, coughing, and sneezing may be painful but this will improve with time. Place a pillow around your incision while sneezing or coughing as this helps to relieve pain.
- It will take time to resume your normal routine. Start by taking short walks and increase your physical activity gradually.
- Avoid operating heavy machinery or driving if you are taking heavy narcotic pain medications that cause drowsiness and slow reaction time.
Wound care: Follow your doctor’s instructions on when you can shower. You should:
- Wash your wound with soap and water and keep it dry.
- Pat dry the wound, instead of rubbing it dry.
- Use a thin pad or gauze to cover the wound, if required.
- Avoid wearing tight clothes to prevent friction near the wound.
- Avoid applying creams or lotions over the wound.
Diet:
- Include more proteins in your meal every day.
- Eat small, frequent meals.
- Follow your doctor’s instruction on fluid consumption to avoid dehydration.
- Slowly include new foods in your diet.
- Avoid foods that can cause gas, loose motions or constipation.
You can resume work when you can work around the house for 8 hours and feel fine the next morning after waking up.
When to see the doctor?
Visit your doctor immediately if you have the following symptoms:
- Black or tarry stools or blood in stools.
- Heaviness in the rectum
- Fever >101°F (38.3°C) that remains even after taking medicine
- Vomiting
- Inability to retain food
- Swelling or pain in the abdomen
- No bowel movements in four days of leaving the hospital
- Normal bowel movements that suddenly stop
- Leakage from the rectum
- Redness, pain and swelling around your incision
- Edges of the incision coming apart
- Chest pain
- Breathlessness
What are the possible complications/risks of proctocolectomy?
The possible complications of proctocolectomy are:
- Chances of infertility and impotence
- Bleeding during the surgery
- Wound infection
- Injury to the ureters (tubes that carry urine from the kidneys to the bladder)
- Incisional hernia a bulge occurring at or near the incision site
- Injury to the nerves that control urethral and reproductive functions
- Intra-abdominal abscess (collection of pus and infected fluid within inflamed tissue in the abdomen)
- Blockage in the ileum
When to follow up with your doctor after a proctocolectomy?
A follow-up visit to your doctor will be arranged in two weeks after your surgery to monitor the healing.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Find Gastroenterologist in cities
- Gastroenterologist in Gurgaon
- Gastroenterologist in Bangalore
- Gastroenterologist in Chennai
- Gastroenterologist in Jaipur
- Gastroenterologist in Ahmedabad
- Gastroenterologist in Noida
- Gastroenterologist in Mysore
- Gastroenterologist in Visakhapatnam
- Gastroenterologist in Hyderabad
- Gastroenterologist in Pune
Surgery Cost In Your City
Doctors for Proctocolectomy

Dr. Rishabh Gupta
Gastroenterology
6 Years of Experience

Dr. Paramjeet Singh.
Gastroenterology
10 Years of Experience

Dr. Nikhil Bhangale
Gastroenterology
10 Years of Experience

Dr Jagdish Singh
Gastroenterology
12 Years of Experience
References
- Crohn's and Colitis Foundation [Internet]. New York. US; Proctocolectomy and Colectomy
- Seer Training: National Cancer Institute [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Small & large intestine
- Canterbury District Health Board [Internet]. New Zealand, Pan Proctocolectomy
- Buie WD, Maclean AR. Proctocolectomy for inflammatory bowel disease–open. In: O’Connell PR, Madoff RD, Solomon MJ, eds. Operative surgery of the colon, rectum and anus. 6th ed. CRC Press; 2015. p. 523-532.
- NYU Langone Health [Internet]. NYU Langone Medical Center. US; Surgery for Inflammatory Bowel Disease in Adults
- Bauer VP. Ileoanal anastomosis (straight and J pouch). In: Townsend CM, Evers BM, eds. Atlas Of general surgical techniques. 1st edition. Philadelphia: Elsevier Saunders; 2010. p. 714.
- Society of American Gastrointestinal and Endoscopic Surgeons [Internet]. California. US; About Conventional Colon Surgery
- UCSF Department of Surgery [internet]. University of California San Francisco. California. U.S.A.; Proctocolectomy
- Cleveland Clinic. [Internet]. Cleveland. Ohio. US; Ileal Pouches
- Dozois EJ. Proctocolectomy and brooke ileostomy for chronic ulcerative colitis. Clin Colon Rectal Surg. 2004;17(1):65‐70. PMID: 20011286.
- Mahmoud NN, Bleier JIS, Aarons CB, Paulson EC, Shanmugen S, Fry RD. Colon and rectum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. [link]. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 51.
- Smith SF, Duell DJ, Martin BC, Gonzalez L, Aebersold M. Perioperative care. In: Smith SF, Duell DJ, Martin BC, Gonzalez L, Aebersold M, eds. Clinical Nursing Skills: Basic to Advanced Skills. 9th ed. New York, NY: Pearson; 2016:chap 26.