Speaking to nephrologist
After the diagnosis, you will visit a nephrologist (Kidney specialist) to check your fitness for a transplant. Initially, questions regarding financial ability will be asked and important information will be provided to you and your family members. This is to ensure that you are aware of the expenses and details of the treatment beforehand. If you are already on dialysis then your dialysis team will work together with your doctors throughout the transplant stages.
Getting tested
You will undergo multiple sets of tests long before your preparation for the operation. It’s a time-consuming process (takes months) and usually takes place in an out-patient setting. Your reports will be thoroughly reviewed, analysed, and discussed to ensure there are no potential complications, during or after the procedure.
These tests are done to rule out any obstructions to successful transplant surgery. The tests include:
Finding a donor
Finding a donor is the most difficult yet crucial stage to get a kidney transplant done. Two types of donors may be chosen:
- Living Donor
You may either have a friend or a family member who might be willing to donate a kidney and are potentially a good match. They will have to undergo a similar, lengthy health examination to make sure they are fit for donation.
- Deceased Donor
A deceased donor is a person who has just died (brain dead) for example, a healthy donor who was taken off the life support system or had a sudden death.
Waiting List
Once your tests indicate you are fit for the transplant, your name will be added to a waiting list for getting the organs from deceased donors if living donors are not available.
In a process called “cross-matching”, your doctor will test the blood from the donor against your blood to predict your immune system’s acceptance of the organ from the donor and avoid transplant rejection.
Meeting the transplant team
A team of surgeons, nephrologists, nurses, social workers, nutritionists and financial coordinators will foresee your treatment and adequate medical care. This will be coordinated by a transplant coordinator who will follow up on your referrals, reports and clinical findings by the team.
To ensure you have a thorough knowledge of the entire procedure, do speak to your doctor and clear your doubts and get answers to all your queries.
Preparations right before surgery
Certain instructions will be given to you by your nurse/doctor, which you must follow before the operation, such as stopping or taking certain medication, coming empty stomach, quitting alcohol and tobacco consumption, foods to include in your diet, things to bring to the hospital and so on.
Testing before the operation is an essential part of the preparation for the surgery, which might include evaluation of your status of health, medical history and circumstances at home.
- Medical examination
A detailed history of your medications, supplements, full body check up and a few laboratory tests will be done before the day of your operation. You will be asked to stop eating or drinking (this is to ensure you do not vomit while you are under general anaesthesia) and stop any medication a few hours before surgery.
- Consent
Final consent for surgery and of your knowledge about the risks will be taken prior to the surgery from you or your family member.
- On the day of surgery
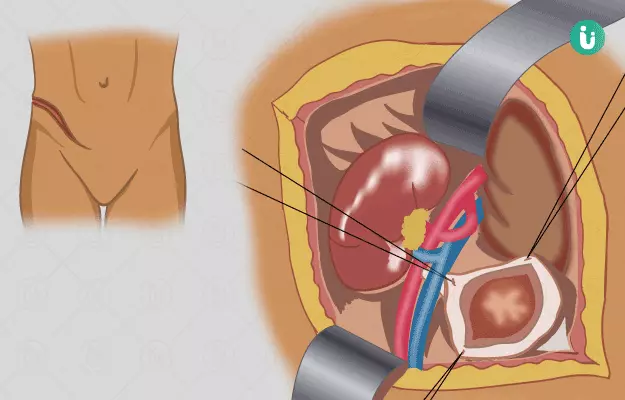
On the day of surgery, you will be given a clean surgical gown/clothes. In the operation theatre, your blood pressure, blood oxygen levels, airway, and heart rate will be monitored.
You will be covered with a germ-free cloth and the site of operation (your belly) will be cleaned with an antiseptic/ antibacterial medicine or solution. This is to ensure proper hygiene and germ-free environment at all times during the operation.