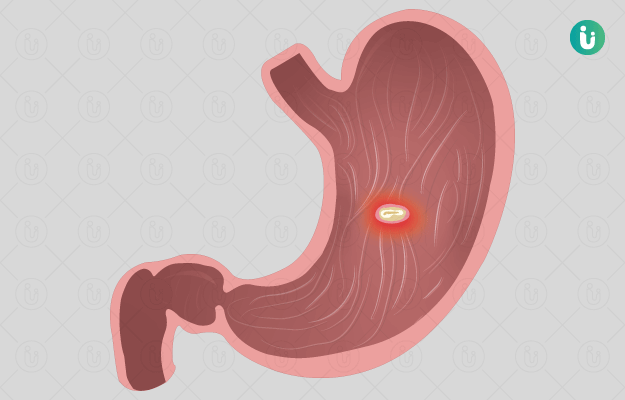
Our skin and mucosal membranes form a protective layer over the body. An ulcer is an open sore or lesion in this protective layer. This opening or discontinuity in the skin or mucosal membrane (inner lining of cavities like the mouth and internal organs like the intestines) impairs the functioning of the affected area and can take a long time to heal.
Ulcers can occur anywhere on or inside the body. Bedsores, genital ulcers, peptic ulcers, leg and foot ulcers, anal fissures and ulcers, corneal ulcers, venous ulcers and mouth ulcers are all ulcers in different parts of the body.
Ulcers tend to be painful, and they can recur. For example, some people who are prone to mouth ulcers keep getting them over and over again.
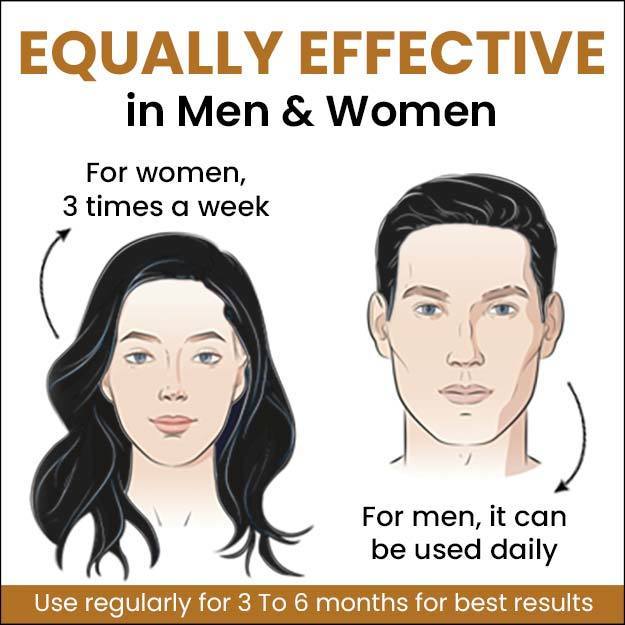
Some chronic conditions and lifestyle habits make people more susceptible to some types of ulcers. For example, people with diabetes are more likely to get foot ulcers (diabetic foot ulcer), people who smoke or take non-steroidal anti-inflammatory drugs (NSAIDs) regularly have a greater chance of developing peptic ulcers (that affect the digestive tract) and people who bite the inside of their cheek are prone to more mouth ulcers. (Read more: Home remedies for mouth ulcers)
The causes of an ulcer can vary from sexually transmitted infections to a wound that takes a long time to heal. For example, bedsores, also called pressure ulcers, can occur when someone lies in bed on the same side for several hours every day or if they have a cast around a broken bone for some weeks.
Whether they are on the outer surfaces of the body (for example, bedsore or leg or foot ulcers) or inside the body (example, peptic ulcers or anal ulcers), ulcers need to be looked over by a doctor. The reason: while some ulcers go away on their own or with over-the-counter medication, others can point to serious underlying health issues and require proper treatment.
Read on to know about the different types of ulcers, ulcer symptoms, ulcer causes, how to prevent an ulcer, ulcer diagnosis and treatment for ulcers:

 Doctors for Ulcer
Doctors for Ulcer  OTC Medicines for Ulcer
OTC Medicines for Ulcer
 Ulcer articles
Ulcer articles

























 Editorial Team
Editorial Team