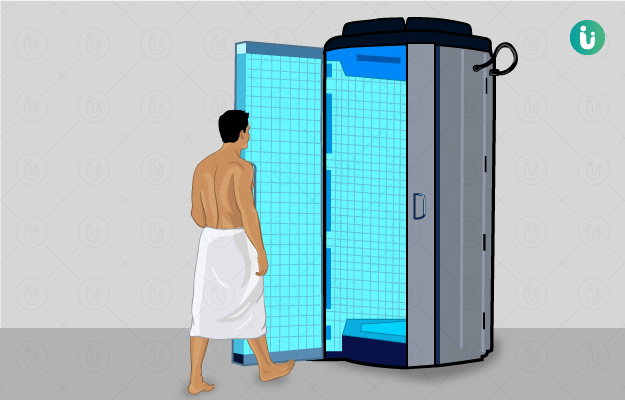
Radiation therapy is a type of therapy that uses the energy of ionising radiation to kill abnormal, usually cancer, cells. Although it is also used in the treatment of non-malignant (not cancerous) conditions, its main use is in the treatment of cancer. Cancer radiation therapy can be used as curative, adjuvant, neoadjuvant or palliative therapy and is usually administered in conjunction with chemotherapy. The doctors that specialise in cancer radiation therapy are called radiation oncologists. The radiation oncologist decides the requirement, dosage, frequency and duration of the cancer radiation therapy required based on the type, stage and extent of cancer. After the decision has been made to subject the patient to cancer radiation therapy, a radiation simulation is conducted. The patient is made to lie on a table and their position is adjusted such that the linear accelerator machine is able to aim optimum ionising emission beams to the tumour. The skin overlying the target spot in this position is marked with a small tattoo. Usually, each radiation therapy session lasts 10 to 30 minutes. Side effects after cancer radiation therapy are expected to arise but normally disappear two months after completion of therapy. However, some may persist for longer.
(Read more: Difference between tumour and cancer)