In diabetes insipidus (DI), due to the decreased secretion or reduced sensitivity to the effects of antidiuretic hormone (ADH), excessive fluid is lost in the urine and the patient experiences increased thirst. Diabetes insipidus symptoms are polyuria (increased frequency and output of urine) and polydipsia (increased thirst and water intake). Other diabetes insipidus symptoms are dehydration and electrolyte imbalance, which can also prove fatal. The underlying diabetes insipidus causes influence the presentation. Diagnosis is made by taking a thorough medical history, conducting a physical examination, laboratory investigations, radiological imaging, and some special tests. Diabetes insipidus treatment includes fluid and electrolyte correction followed by desmopressin in some cases of central diabetes insipidus. The overall outlook is good; however, electrolyte imbalance can be deadly.
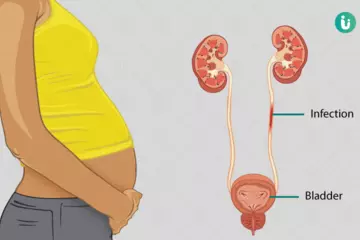
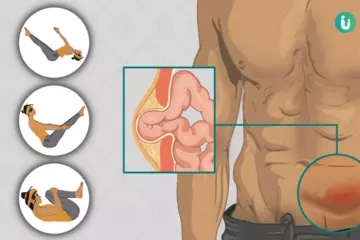
Diuresis is the technical term that refers to the excessive production of urine by the kidneys due to the filtration of extra body fluids. ADH, also known as arginine vasopressin (AVP), is synthesized by the hypothalamus and is released by the pituitary gland, along with oxytocin, through its posterior lobe. Vasopressin, by binding with V2 receptors in the distal convoluted tubules (DCT) of the kidneys, increases water permeability and resorption of extra fluid. Thus, by reducing the urine output, it exerts an antidiuretic effect. When a person is dehydrated or thirsty, the vasopressin level is raised by the central nervous system (hypothalamus and pituitary gland) and this causes more water to be absorbed back from the urine (which becomes more concentrated and dark) in the kidneys. Similarly, when a person is adequately hydrated and has had enough to drink, the vasopressin levels are down-regulated by the same organs and more water is allowed to leave the body through urine (which becomes diluted and pale).
Please visit this site for complete diabetes treatment.
Certain conditions can produce central diabetes insipidus (DI), where the synthesis or secretion of ADH is reduced significantly. In other cases, due to underlying causes, the V2 vasopressin (ADH) receptors in the distal convoluted tubules (DCT) of the kidney can become insensitive to the hormone. That is to say, the receptor molecules do not bind with the hormone molecule and the physiological change necessary for the fluid to be absorbed back into the circulatory system of the body does not occur.
In this article, you will get information about diabetes insipidus symptoms, causes, and treatment.
(Read More - Diabetic Nephropathy treatment)

 Doctors for Diabetes Insipidus
Doctors for Diabetes Insipidus  OTC Medicines for Diabetes Insipidus
OTC Medicines for Diabetes Insipidus